New Study May Impact Practice Guidelines for Mitral Valve Surgery for Severe Ischemic Mitral Regurgitation
New findings showing mitral valve replacement may be more effective than mitral valve repair reported at AHA Scientific Sessions 2013 and in New England Journal of Medicine.
The Cardiothoracic Surgical Trials Network (CTSN), whose Data and Clinical Coordinating Center is at Icahn School of Medicine at Mount Sinai, is reporting for the first time evidence on whether or not there is any significant difference between the two current surgical approaches to treat patients with severe ischemic mitral regurgitation — mitral valve repair and mitral valve replacement.
The findings presented on November 18 at the American Heart Association’s Scientific Sessions 2013 and published simultaneously by the New England Journal of Medicine, report similar clinical outcomes one-year following mitral valve surgery for both surgical approaches. Although patient clinical outcomes were similar, mitral valve replacement was shown to be more durable than repair.
"Ischemic mitral regurgitation is an important public health problem affecting as many as two million Americans. Our study is the first definitive clinical trial to address the relative merits of mitral valve repair versus mitral valve replacement surgery in patients suffering from severe ischemic mitral regurgitation,” says Annetine C. Gelijns, PhD, Professor and Chair of the Department of Health Evidence and Policy at Icahn School of Medicine at Mount Sinai, who is the corresponding author for the NEJM study and principal investigator for the Data and Clinical Coordinating Center based at Mount Sinai for the NIH-sponsored Cardiothoracic Surgical Trials Network (CTSN) which conducted the clinical trial study.
Ischemic mitral regurgitation occurs when blood backflows into the left atrium from the left ventricle of the heart due to improper closure of the mitral valve. The condition often develops as a complication from a heart attack and subsequent enlargement of the left ventricle, the heart's main pumping chamber. If not surgically corrected, the condition has been reported to potentially have a one-year mortality risk as high as 40 percent.
Currently, practice guidelines recommend valve repair or replacement for severe ischemic mitral regurgitation. However, lack of evidence has led to uncertainty and variation in surgical practice, although surgeons' use of repair has increased over time.
Previous research has shown mitral valve repair has lower operative mortality and complications, while mitral valve replacement may provide better long-term correction of mitral regurgitation.
"These results may impact the surgical care of patients experiencing severe ischemic mitral regurgitation and offer the strongest evidence to date to inform future surgical practice guidelines,” says Michael K. Parides, PhD, Professor of Biostatistics in the Department of Health Evidence and Policy at Icahn School of Medicine at Mount Sinai, the principal statistician for the CTSN.
This multicenter, randomized clinical trial included 22 clinical centers in North America randomizing 251 patients. It evaluated the safety and effectiveness of mitral valve repair and mitral valve replacement in patients with severe ischemic mitral regurgitation. Comparative effectiveness was based on the degree of left ventricular remodeling, mortality, adverse events, recurrent mitral regurgitation, hospitalizations, and quality of life one-year after surgery.
"While our study results clearly demonstrate that patient outcomes with replacement and repair are similar one-year after surgery, our ongoing patient follow-up is extremely important, as it will reveal any consequences for patients whose mitral regurgitation has recurred,” says Alan J. Moskowitz, MD, Professor and Vice-Chair of the Department of Health Evidence and Policy at Icahn School of Medicine at Mount Sinai and study co-author.
The CTSN has eight core clinical centers in the U.S. and Canada. The CTSN Data and Clinical Coordinating Center, based at Icahn School of Medicine at Mount Sinai, directs each of its clinical trial's design, methodologies, ethical research concerns, study data, analysis, and reporting.
As principal investigator for CTSN's Data and Clinical Coordinating Center based at Mount Sinai, Dr. Gelijns previously received financial compensation as a consultant for InHealth's Research Council, a not-for-profit agency which has supported some of the study-related analyses.
This study was presented as the Late-Breaking Clinical Trial (Abstract 19636): Severe Ischemic Mitral Regurgitation: Is it Better to Repair or Replace the Valve?
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
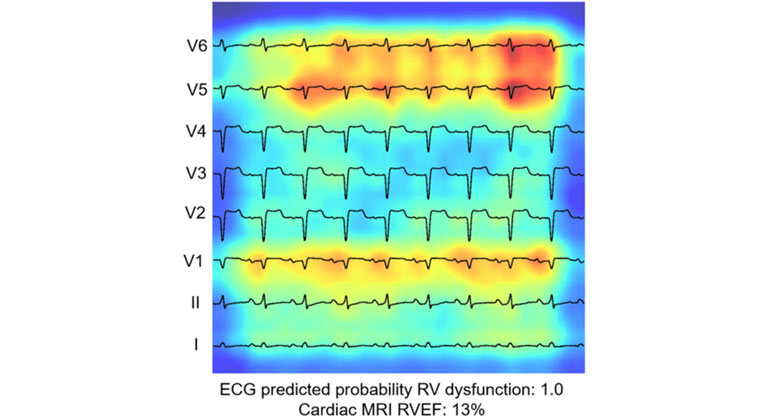
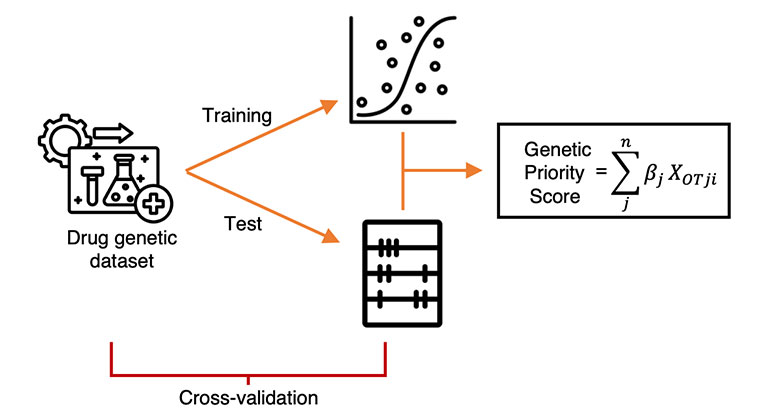
AI-Driven Study Redefines Right Heart Health Assessment With Novel Predictive Model
Jan 04, 2024 View All Press Releases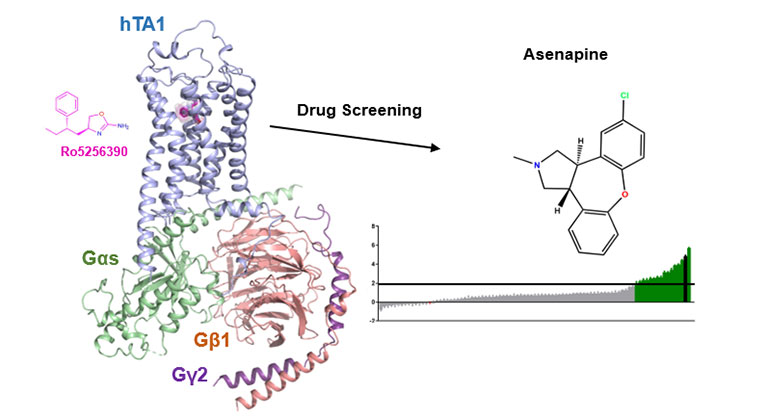
Demystifying a Key Receptor in Substance Use and Neuropsychiatric Disorders
Jan 02, 2024 View All Press Releases