Typhoid fever
Enteric fever
Typhoid fever is an infection that causes fever, diarrhea, and a rash. It is most commonly caused by bacteria called Salmonella typhi (S typhi).
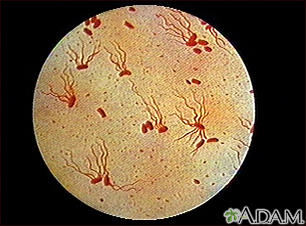
The causative agent of typhoid fever is the bacterium Salmonella typhi. (Image courtesy of the Centers for Disease Control and Prevention.)
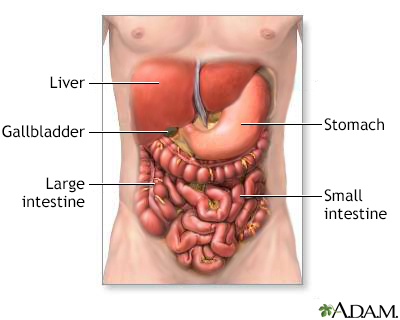
The digestive system organs in the abdominal cavity include the liver, gallbladder, stomach, small intestine and large intestine.
Causes
S typhi is spread through contaminated food, drink, or water. If you eat or drink something that is contaminated with the bacteria, the bacteria enter your body. They travel into your intestines, and then into your blood. In the blood, they travel to your lymph nodes, gallbladder, liver, spleen, and other parts of the body.
Some people become carriers of S typhi and continue to release the bacteria in their stools, sometimes for years, spreading the disease.
Typhoid fever is common in developing countries. Most cases in the United States are brought in from other countries where typhoid fever is common.
Symptoms
Early symptoms include fever, general ill-feeling, and abdominal pain. High fever (103°F, or 39.5°C) or higher and severe diarrhea occur as the disease gets worse.
Some people develop a rash called "rose spots," which are small red spots on the abdomen and chest.
Other symptoms that occur include:
- Bloody stools
- Chills
- Agitation, confusion, delirium, seeing or hearing things that are not there (hallucinations)
- Difficulty paying attention (attention deficit)
- Nosebleeds
- Severe fatigue
- Slow, sluggish, weak feeling
Exams and Tests
Your health care provider will perform a physical exam and ask about the symptoms.
A complete blood count (CBC) will show a high number of white blood cells.
A blood culture during the first week of the fever can show S typhi bacteria.
Other tests that can help diagnose this condition include:
- ELISA blood test to look for antibodies to the S typhi bacteria
- Fluorescent antibody study to look for substances that are specific to S typhi bacteria
- Platelet count (platelet count may be low)
- Stool culture
Treatment
Fluids and electrolytes may be given by IV (into a vein) or you may be asked to drink water with electrolyte packets.
Antibiotics are given to kill the bacteria. There are increasing rates of antibiotic resistance throughout the world, so your provider will check current recommendations before choosing an antibiotic.
Outlook (Prognosis)
Symptoms usually improve in 2 to 4 weeks with treatment. The outcome is likely to be good with early treatment, but becomes poor if complications develop.
Symptoms may return if the treatment has not completely cured the infection.
Possible Complications
Health problems that may develop include:
- Intestinal hemorrhage (severe GI bleeding)
- Intestinal perforation
- Kidney failure
- Peritonitis
When to Contact a Medical Professional
Contact your provider if you have any of the following:
- You know you have been exposed to someone who has typhoid fever
- You have been in an area where there are people who have typhoid fever and you develop symptoms of typhoid fever
- You have had typhoid fever and the symptoms return
- You develop severe abdominal pain, decreased urine output, or other new symptoms
Prevention
A vaccine is recommended for travel outside of the United States to places where there is typhoid fever. The Centers for Disease Control and Prevention website has information about where typhoid fever is common --
When traveling, drink only boiled or bottled water and eat well-cooked food. Wash your hands thoroughly before eating.
Water treatment, waste disposal, and protecting the food supply from contamination are important public health measures. Carriers of S typhi must not be allowed to work as food handlers.
References
Andrews JR, Harris JB, Ryan ET. Typhoid fever, paratyphoid fever, and typhoidal fevers. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 100.
Melia JMP, Sears CL. Infectious enteritis and proctocolitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 110.
Version Info
Last reviewed on: 5/19/2023
Reviewed by: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
