How to care for pressure sores
Pressure ulcer - care; Bedsore - care; Decubitus ulcer - care
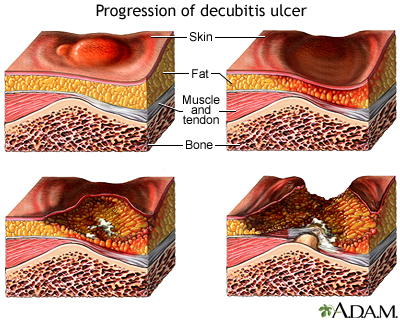
If untreated, a pressure sore can progress from a small irritated but unbroken skin patch to a potentially life-threatening wound involving extensive tissue death and infection. Treatment of the serious decubitus ulcer may include debriding (excising) the dead tissue and administering systemic antibiotics.
Causes
Pressure sores occur when there is too much pressure on the skin for too long. This reduces blood flow to the area. Without enough blood to nourish the skin, the skin can die and a sore may form.
You are more likely to get a pressure sore if you:
- Use a wheelchair or stay in bed for a long time
- Are an older adult
- Cannot move certain parts of your body without help
- Have a disease that affects blood flow, including diabetes or vascular disease
- Have Alzheimer disease or another condition that affects your mental state
- Have fragile skin
- Cannot control your bladder or bowels
- Do not get enough nutrition
Symptoms
Pressure sores are grouped by the severity of symptoms. Stage I is the mildest stage. Stage IV is the worst.
- Stage I: A reddened, painful area on the skin that does not turn white (blanch) when pressed. This is a sign that a pressure ulcer may be forming. The skin may be warm or cool, firm or soft.
- Stage II: The skin blisters or forms an open sore. The area around the sore may be red and irritated.
- Stage III: The skin now develops an open, sunken hole called a crater or ulcer. The tissue below the skin is damaged. You may be able to see body fat in the ulcer.
- Stage IV: The pressure ulcer has become so deep that there is damage to the muscle and bone, and sometimes to tendons and joints.
There are two other types of pressure sores that don't fit into the stages.
- Sores covered in dead skin that is yellow, tan, green, or brown. The dead skin makes it hard to tell how deep the sore is. This type of sore is unstageable.
- Pressure sores that develop in the tissue deep below the skin. This is called a deep tissue injury. The area may be dark purple or maroon. There may be a blood-filled blister under the skin. This type of skin injury can quickly become a stage III or IV pressure sore.
Pressure sores tend to form where skin covers bony areas with less tissue under the skin to pad the area. These include:
- Buttocks
- Elbow
- Hips
- Heels
- Ankles
- Shoulders
- Back
- Back of head
Caring for a Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here's how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should move or be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
- For a stage I sore, you can wash the area gently with mild soap and water. If needed, use a moisture barrier to protect the area from bodily fluids. Ask your provider what type of moisture barrier to use.
- Stage II pressure sores should be cleaned with a salt water (saline) rinse to remove loose, dead tissue. Or, your provider may recommend a specific cleanser.
- Do not use hydrogen peroxide or iodine cleansers unless directed by your provider as they can damage the skin.
- Keep the sore covered with a dressing. This protects against infection and helps keep the sore moist so it can heal.
- Talk with your provider about what type of dressing to use. Depending on the size and stage of the sore, you may use a film, gauze, gel, foam, or other type of dressing.
- Most stage III and IV sores will be treated by your provider. Ask about any special instructions for home care.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn't rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can't see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
- Eat healthy foods. Getting the right nutrition will help you heal.
- Lose excess weight.
- Get plenty of sleep.
- Ask your provider if it's OK to do gentle stretches or light exercises. This can help improve circulation.
Do not massage the skin near or on the ulcer. This can cause more damage. Do not use donut-shaped or ring-shaped cushions. They reduce blood flow to the area, which may cause sores.
When to Call the Doctor
Contact your provider if you develop blisters or an open sore.
Call immediately if there are signs of infection, such as:
- A foul odor from the sore
- Pus coming out of the sore
- Redness and tenderness around the sore
- Skin close to the sore is warm and/or swollen
- Fever
References
James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM. Dermatoses resulting from physical factors. In: James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM, eds. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 3.
Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2015;162(5):370-379. PMID: 25732279
Woelfel SL, Armstrong DG, Shin L. Wound care. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 118.
Version Info
Last reviewed on: 4/9/2024
Reviewed by: Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
