Treating an Enlarged Prostate With an Interventional Radiology Procedure Is Life-Changing
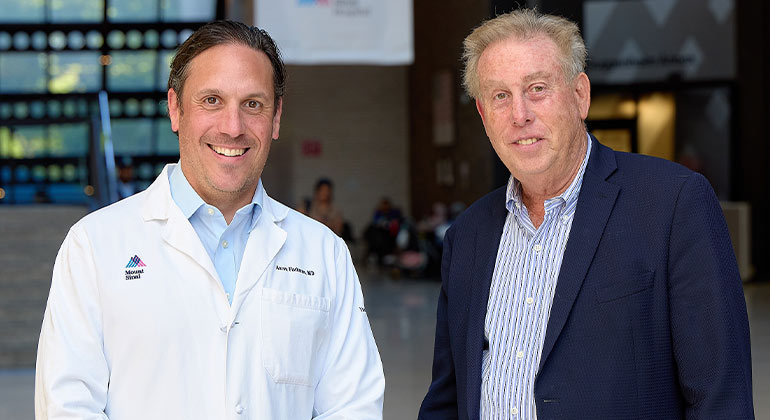
Norman Solomon, 69, took a long road to interventional radiologist Aaron Fischman, MD. Norman’s urinary challenges started when he was only 28. “I’m a rare case,” he explains. He was diagnosed with benign prostatic hyperplasia (BPH), or an enlarged prostate, and over the years, he tried a series of doctors and a variety of medications, all to no avail. Ultimately, he reached out to Dr. Fischman and received state-of-the-art treatment that solved the problem.
“Some robotic surgeons encouraged me to have a procedure,” Norman says. “But I didn’t want to because of the possible complications—I feared impotency and running the risk of incontinence.” Eventually, Norman did his own research and discovered the minimally invasive procedure called prostate artery embolization (PAE), a same-day procedure with few, if any, complications. The next step was to find a doctor who did the procedure. His online research led him to Dr. Fischman at The Mount Sinai Hospital.
Dr. Fischman ordered a variety of imaging and blood tests to make sure Norman was a good candidate. “BPH is very common. Basically, when you get older, your prostate gets bigger and bigger. By the time you’re 50, half of all men have BPH. By the time you’re 80 years old, 80 percent of men have it,” he explains. “What happens when your prostate gets bigger is that it is harder to urinate; the urine comes out more slowly, and you’re not always able to fully empty your bladder, which means you make more trips to the bathroom.”
Years ago, the medical response was to remove the prostate completely. But, since BPH is benign—not cancerous—it is not necessary to take such a radical approach, Dr. Fischman explains. A variety of medications and surgical approaches can improve the symptoms. For some patients, a good option is PAE, which is a complex procedure, performed by interventional radiologists that can produce excellent results. “If you pick the right patients, you have an 85 to 90 percent success rate,” says Dr. Fischman, Professor of Diagnostic, Molecular and Interventional Radiology, Urology, and Surgery at the Icahn School of Medicine at Mount Sinai.
“We insert a very, very thin catheter through the wrist,” he says. “Then, using an X-ray, we guide the catheter into the artery that supplies the blood to the prostate. We insert a substance—usually a type of gelatin or glue—that occludes, or blocks, the blood vessels so the prostate gets less blood.” Over time, the prostate shrinks, and the urine channel opens up. “It’s much less invasive than any of the other options,” he adds.
The outpatient procedure itself takes about an hour, though Norman was in the hospital for three or four hours. He took it easy for the rest of the day, but by the next day, Norman was back at work. He didn’t feel relief right away, though. Dr. Fischman explains, “When you cut off the blood flow to the prostate, it starts to shrink, but it doesn’t immediately get smaller. It can take weeks to months for that to occur. Also, the body has to adjust to having a lower blood flow to the prostate, which can take a little time.”
Now, about a year after the procedure, Norman says his symptoms were 90 percent gone. “It was completely life changing. I can fly to Dallas and sit in the middle seat,” he jokes. And Norman has only good things to say about the experience. “Dr. Fischman couldn’t have been more comforting and professional. The entire team gets an A+. There was not a single negative to deal with,” Norman says.