Gastroesophageal reflux - discharge
Peptic esophagitis - discharge; Reflux esophagitis - discharge; GERD - discharge; Heartburn - chronic - discharge
Gastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backwards from the stomach into the esophagus (the tube from the mouth to the stomach). It is common to have acid reflux once in a while. If it happens often and causes bothersome symptoms, it is called GERD. This article tells you what you need to do to manage your condition.
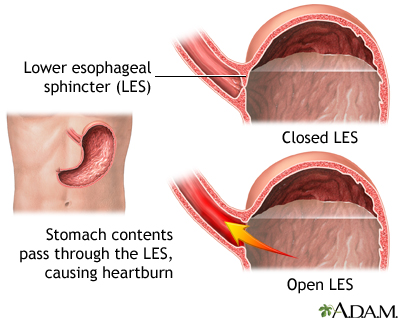
A band of muscle fibers, the lower esophageal sphincter, closes off the esophagus from the stomach. If the sphincter does not close properly, food and liquid can move backward into the esophagus and cause heartburn and other symptoms known as gastroesophageal disease (GERD). To alleviate symptoms dietary changes and medications are prescribed. For a patient who has persistent symptoms despite medical treatment, an anti-reflux operation may be an option.
Self-care
You can make many lifestyle changes to help treat your symptoms. Avoid foods that cause problems for you.
- Do not drink alcohol.
- Do not smoke.
- Avoid drinks and foods that have caffeine, such as soda, coffee, tea, and chocolate.
- Avoid decaffeinated coffee. It also increases the level of acid in your stomach.
- Avoid high-acid fruits and vegetables, such as citrus fruits, pineapple, tomatoes, or tomato-based dishes (pizza, chili, and spaghetti) if you find that they cause heartburn.
- Avoid items with spearmint or peppermint.
Other lifestyle tips that may make your symptoms better are:
- Eat smaller meals, and eat more often.
- Lose weight, if you need to.
- If you smoke or chew tobacco, try to quit. Your health care provider can help.
- Exercise, but not right after eating.
- Reduce your stress and watch for stressful, tense times. Stress can bother your reflux problem.
- Bend at the knees, not your waist, to pick things up.
- Avoid wearing clothes that put pressure on your waist or stomach.
- Do not lie down for 3 to 4 hours after eating.
- Raise the head of your bed 4 to 6 inches (10 to 15 centimeters).
Avoid medicines such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn). Take acetaminophen (Tylenol) to relieve pain. Take any of your medicines with plenty of water. When you start a new medicine, remember to ask if it will make your heartburn worse.
Try these tips before going to sleep:
- Do not skip meals or eat a large meal for dinner to make up for missed meals.
- Avoid late night snacks.
- Do not lie down right after you eat. Remain upright for 3 to 4 hours after your last meal before you go to bed.
- Raise the head of your bed 4 to 6 inches (10 to 15 centimeters), using blocks. You can also use a wedge support that raises the top half of your body when you are in bed. Extra pillows that raise only your head may not help.
Drug Treatment
Antacids can help neutralize your stomach acid. They can help with the symptoms of GERD but do not help to treat the irritation in your esophagus. Common side effects of antacids include diarrhea or constipation.
Other over-the-counter medicines and prescription medicines can treat GERD. They work more slowly than antacids but give you longer relief. Your provider can tell you how to take these medicines. There are 3 different types of these medicines:
- H2 antagonists: famotidine (Pepcid, Zantac), cimetidine (Tagamet), and nizatidine (Axid)
- Proton pump inhibitors (PPI): omeprazole (Prilosec or Zegarid), esomeprazole (Nexium), lansoprazole (Prevacid), dexlansoprazole (Dexilant), rabeprazole (AcipHex), and pantoprazole (Protonix)
- Potassium-competitive acid blockers (P-CABs) (vonoprazan and tegoprazan)
Follow-up
You will have follow-up visits with your provider to discuss your symptoms. If you had complications of GERD such as moderate-to-severe erosive esophagitis, you may need to stay on long-term medicines. If you have Barrett esophagus, you will be entered into surveillance with upper endoscopy at certain intervals. If symptoms continue, other testing may be needed. Some surgical procedures may offered depending on your particular situation. You may also need to have dental check-ups. GERD can cause the enamel on your teeth to wear away.
When to Call the Doctor
Contact your provider if you have:
- Problems or pain with swallowing
- Choking
- A full feeling after eating a small meal portion
- Weight loss that cannot be explained
- Vomiting
- Loss of appetite
- Chest pain
- Bleeding, blood in your stools, or dark, tarry looking stools
- Hoarseness
References
Abdul-Hussein M. Gastroesophageal reflux disease (GERD). In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:230-233.
Falk GW, Katzka DA. Diseases of the esophagus. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 124.
Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117(1):27-56. PMID: 34807007
Patel A, Laine L, Moayyedi P, Wu J. AGA Clinical practice update on integrating potassium-competitive acid blockers into clinical practice: Expert review. Gastroenterology. 2024:167(6):1228-1238. PMID: 39269391
Richter JE,Vaezi MF. Gastroesophageal reflux disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 46.
Version Info
Last reviewed on: 10/30/2024
Reviewed by: Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
