Albinism
Oculocutaneous albinism; Ocular albinism
Albinism is a lack of melanin production. Melanin is a natural substance in the body that gives color to your hair, skin, and iris of the eye.
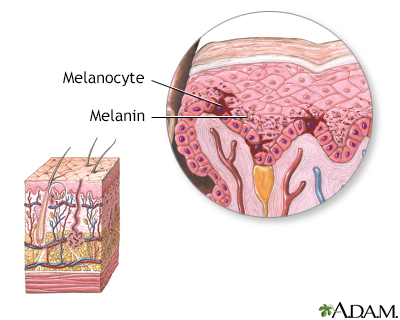
Melanin is the natural substance that gives color (pigment) to hair, skin, and the iris.
Causes
Albinism occurs when one of several genetic changes makes the body unable to produce or distribute melanin.
These changes may be passed down (inherited) through families.
The most severe form of albinism is called oculocutaneous albinism. People with this type of albinism have white or pink hair, skin, and iris color. They also have vision problems.
Another type of albinism, called ocular albinism type 1 (OA1), affects only the eyes. The person's skin and eye color are usually in the normal range. However, an eye exam will show that there is no coloring in the back of the eye (retina).
Hermansky-Pudlak syndrome (HPS) is a form of albinism caused by a change to a single gene. It can occur with a bleeding disorder, as well as with lung, kidney, and bowel diseases.
Symptoms
A person with albinism may have one of these symptoms:
- No color in the hair, skin, or iris of the eye
- Lighter than normal skin and hair
- Patches of missing skin color
Many forms of albinism are associated with the following symptoms:
- Crossed eyes
- Light sensitivity
- Rapid eye movements
- Vision problems, or functional blindness
Exams and Tests
Genetic testing offers the most accurate way to diagnose the specific type of albinism. Such testing is helpful if you have a family history of albinism. It is also useful for certain groups of people who are known to get the disease.
Your health care provider may also diagnose the condition based on the appearance of your skin, hair, and eyes. An eye doctor called an ophthalmologist may perform an electroretinogram. This is a test that can reveal vision problems related to albinism. A test called a visual evoked potentials test can be very useful when the diagnosis is uncertain.
Treatment
The goal of treatment is to relieve symptoms. It will depend on how severe the disorder is.
Treatment involves protecting the skin and eyes from the sun. To do this:
- Reduce sunburn risk by avoiding the sun, using sunscreen, and covering up completely with clothing when exposed to the sun.
- Use sunscreen with a high sun protection factor (SPF).
- Wear sunglasses (UV protected) to help relieve light sensitivity.
Glasses are often prescribed to correct vision problems and eye position. Eye muscle surgery is sometimes recommended to correct abnormal eye movements.
Support Groups
More information and support for people with albinism and their families can be found at:
- National Organization for Albinism and Hypopigmentation --
www.albinism.org - National Library of Medicine - MedlinePlus website. Ocular albinism. --
medlineplus.gov/genetics/condition/ocular-albinism/
Outlook (Prognosis)
Albinism does not usually affect lifespan. However, the HPS form of albinism can shorten a person's lifespan due to lung disease or bleeding problems.
People with albinism may be limited in their outdoor activities because they can't tolerate the sun.
Possible Complications
These complications can occur:
- Decreased vision, blindness
- Skin cancer
When to Contact a Medical Professional
Contact your provider if you have albinism or symptoms such as light sensitivity that cause discomfort. Also contact your provider if you notice any skin changes that might be an early sign of skin cancer.
Prevention
Because albinism is inherited, genetic counseling is important. People with a family history of albinism or very light coloring should consider genetic counseling.
References
Joyce JC. Hypopigmented lesions. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 694.
Nischal KK. Ophthalmology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 20.
Paller AS, Mancini AJ. Disorders of pigmentation. In: Paller AS, Mancini AJ, eds. Paller and Mancini - Hurwitz Clinical Pediatric Dermatology. 6th ed. St Louis, MO: Elsevier; 2022:chap 11.
Version Info
Last reviewed on: 12/31/2023
Reviewed by: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
