Ankylosing spondylitis
Spondylitis; Spondyloarthritis; HLA - B27
Ankylosing spondylitis (AS) is a chronic form of arthritis. It mostly affects the bones and joints at the base of the spine where it connects with the pelvis. These joints can become swollen and inflamed. Over time, the affected spinal bones may join together.
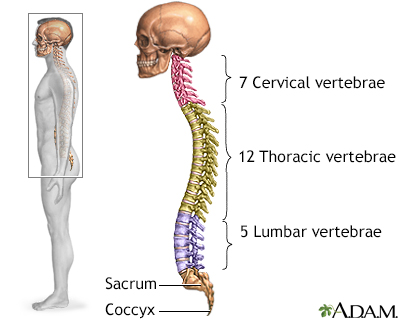
The spine is divided into several sections. The cervical vertebrae make up the neck. The thoracic vertebrae comprise the chest section and have ribs attached. The lumbar vertebrae are the remaining vertebrae below the last thoracic bone and the top of the sacrum. The sacral vertebrae are caged within the bones of the pelvis, and the coccyx represents the terminal vertebrae or vestigial tail.
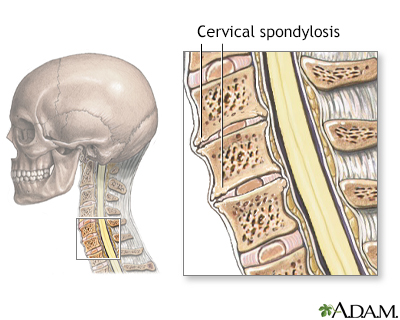
Cervical spondylosis is a disorder that results from abnormal growth of the bones of the neck and degeneration and mineral deposits in the cushions between the vertebrae. Progressive neck pain is a key indication of cervical spondylosis. It may be the only symptom in many cases. Examination often shows limited ability to bend the head toward the shoulders and limited ability to rotate the head. The goal of treatment is relief of pain and prevention of permanent spinal cord and nerve root injury.
Causes
AS is the main member of a family of similar forms of arthritis called spondyloarthritis. Other members include psoriatic arthritis, arthritis of inflammatory bowel disease and reactive arthritis. This family of arthritis affects up to 1 in 100 people.
The cause of AS is unknown, however genes seem to play a role. The majority of people with AS are positive for the HLA-B27 gene, but not everyone who has this gene has AS.
The disease often begins between ages 20 and 40, but it may begin before age 10. It affects more males than females.
Symptoms
AS starts with lower back pain that comes and goes but usually becomes present most of the time as the condition progresses.
- Pain and stiffness are worse at night, in the morning, or when you are less active. The discomfort may wake you from sleep.
- The pain often gets better with activity or exercise.
- Back pain may begin in the joint between the pelvis and spine (sacroiliac joints). Over time, it may involve all or part of the spine.
- Your lower spine may become less flexible. Over time, you may stand in a hunched forward position.
Other parts of your body that may be affected include:
- The joints of the shoulders, knees and ankles, which may be swollen and painful
- The joints between your ribs and breastbone, so that you cannot expand your chest fully
- The eye, which may have swelling and redness called uveitis
Fatigue is also a common symptom.
Less common symptoms include:
- Slight fever
AS may occur with other conditions, such as:
- Psoriasis
- Ulcerative colitis or Crohn disease
- Recurring or chronic eye inflammation (iritis, uveitis)
Exams and Tests
Tests may include:
- Anti-cyclic citrullinated peptide (CCP) antibody (which should be negative)
- Complete blood count (CBC)
- ESR (a measure of inflammation)
- HLA-B27 antigen (which detects the gene linked to ankylosing spondylitis)
- Rheumatoid factor (which should be negative)
- X-rays of the spine and pelvis
- MRI of the spine and pelvis
Treatment
Your health care provider may prescribe medicines such as non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling and pain.
- Some NSAIDs can be bought over-the-counter (OTC). These include aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve, Naprosyn).
- Other NSAIDs are prescribed by your provider.
- Talk to your provider or pharmacist before daily long-term use of any over-the-counter NSAID.
You may also need stronger medicines to control pain and swelling, such as:
- Corticosteroid therapy (such as prednisone) used for short periods of time
- Sulfasalazine
- A biologic tumor necrosis factor (TNF) inhibitor (such as etanercept, adalimumab, infliximab, certolizumab or golimumab)
- A biologic inhibitor of IL17A, secukinumab
Surgery, such as hip replacement, may be done if pain or joint damage is severe.
Exercises can help improve posture and breathing. Lying flat on your back at night can help you keep a normal posture.
Outlook (Prognosis)
The course of the disease is hard to predict. Over time, signs and symptoms of AS flareup (relapse) and quiet down (remission). Most people are able to function well unless they have a lot of damage to the hips or the spine. Joining a support group of others with the same problem may often help.
Treatment with NSAIDs often reduces the pain and swelling. Treatments given by IV or injection such as TNF inhibitors early in the disease appears to slow progression of the spine arthritis. Other newer drugs such as Interleukin-17 inhibitors and oral medicines, Janus kinase (JAK) inhibitors have been approved as well.
Rarely, people with ankylosing spondylitis may have problems with:
- Psoriasis, a chronic skin disorder
- Inflammation in the eye (uveitis)
- Inflammation in the intestine (colitis)
- Abnormal heart rhythm
- Scarring or thickening of the lung tissue
- Scarring or thickening of the aortic heart valve
- Spinal cord injury after a fall
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of ankylosing spondylitis
- You have ankylosing spondylitis and develop new symptoms during treatment
References
Gardocki RJ, Park AL. Degenerative disorders of the thoracic and lumbar spine. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 39.
Inman RD. The spondyloarthropathies. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 249.
van der Linden S, Brown M, Gensler LS, Kenna T, Maksymowych WP, Taylor WJ. Ankylosing spondylitis and other forms of axial spondyloarthritis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 80.
Ward MM, Deodhar A, Gensler LS, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Care Res (Hoboken). 2019;71(10):1285-1299. PMID: 31436026
Werner BC, Feuchtbaum E, Shen FH, Samartzis D. Ankylosing spondylitis of the cervical spine. In: Shen FH, Samartzis D, Fessler RG, eds. Textbook of the Cervical Spine. Philadelphia, PA: Elsevier Saunders; 2015:chap 28.
Version Info
Last reviewed on: 4/30/2023
Reviewed by: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, New York, NY, and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
