Ataxia - telangiectasia
Louis-Bar syndrome
Ataxia-telangiectasia is a rare childhood disease. It affects the brain and other parts of the body.
Ataxia refers to uncoordinated movements, such as walking. Telangiectasias are enlarged blood vessels (capillaries) just below the surface of the skin. Telangiectasias appear as tiny, red, spider-like blood vessels.
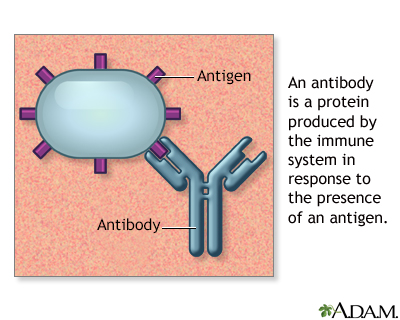
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
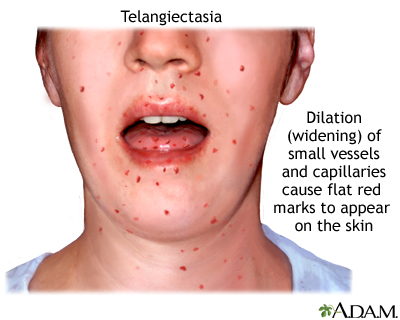
Telangiectasia is the dilation of small superficial vessels and capillaries that cause numerous flat red marks on the hands, face and tongue. Telangiectasia can be a symptom of scleroderma or other systemic diseases.
Causes
Ataxia-telangiectasia is inherited. This means it is passed down through families. It is an autosomal recessive trait. Both parents must provide a copy of a nonworking gene for the child to have symptoms of the disorder.
The disease results from a variant in the ATM gene. This gene provides instructions for making a protein that helps control the rate at which cells grow and divide. Defects in this gene can lead to abnormal cell death in many sites of the body, including the part of the brain that helps coordinate movement.
Boys and girls are equally affected.
Symptoms
Symptoms include:
- Decreased coordination of movements (ataxia) in late childhood that can include ataxic gait (cerebellar ataxia), jerky gait, unsteadiness
- Decreasing mental development, slows or stops after age 10 to 12
- Delayed walking
- Discoloration of skin areas exposed to sunlight
- Discoloration of skin (coffee-with-milk-colored spots)
- Enlarged blood vessels in skin of nose, ears, and inside of the elbow and knee
- Enlarged blood vessels in the whites of the eyes
- Jerky or abnormal eye movements (nystagmus) late in the disease
- Premature graying of the hair
- Seizures
- Sensitivity to radiation, including x-rays
- Severe respiratory infections that keep coming back (recurring)
Exams and Tests
Your health care provider will perform a physical exam. The exam may show signs of the following:
- Tonsils, lymph nodes, and spleen below normal size
- Decreased to absent deep tendon reflexes
- Delayed or absent physical and sexual development
- Growth failure
- Mask-like face
- Multiple skin coloring and texture changes
Possible tests include:
- Alpha fetoprotein
- B and T cell screen
- Carcinoembryonic antigen
- Genetic testing to look for changes in the ATM gene
- Glucose tolerance test
- Serum immunoglobulin levels (IgE, IgA)
- X-ray or CT scan to look at the size of the thymus gland
Treatment
There is no specific treatment for ataxia-telangiectasia. Treatment is directed at specific symptoms.
Support Groups
More information and support for people with ataxia-telangiectasia condition and their families can be found at:
- Ataxia Telangiectasia Children's Project:
www.atcp.org - National Ataxia Foundation (NAF):
www.ataxia.org
Outlook (Prognosis)
Early death is common, but life expectancy varies.
Because people with this condition are very sensitive to radiation, they should never be given radiation therapy, and no unnecessary x-rays should be done.
Possible Complications
Complications may include:
- Cancer, such as lymphoma
- Diabetes
- Kyphosis
- Progressive movement disorder that leads to wheelchair use
- Scoliosis
- Severe, recurrent lung infections
When to Contact a Medical Professional
Contact your provider if your child develops symptoms of this disorder.
Prevention
Couples with a family history of this condition who are considering pregnancy may consider genetic counseling.
Parents of a child with this disorder may have a slight increased risk for cancer. They should have genetic counseling and increased cancer screenings.
References
Cunningham-Rundles C. Primary immunodeficiency diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 231.
Martin KL. Vascular disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 669.
National Center for Advancing Translational Sciences. Genetic and Rare Diseases Information Center website. Ataxia-telangiectasia.
Safier RA, Cleves-Bayon C, Gaesser J. Neurology. In: Zitelli BJ, McIntire SC, Nowalk AJ, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 16.
Version Info
Last reviewed on: 9/18/2023
Reviewed by: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
