Dilated cardiomyopathy
Cardiomyopathy - dilated; Primary cardiomyopathy; Diabetic cardiomyopathy; Idiopathic cardiomyopathy; Alcoholic cardiomyopathy
Cardiomyopathy is disease in which the heart muscle becomes weakened, stretched, or has another structural problem.
Dilated cardiomyopathy is a condition in which the heart muscle becomes weakened and enlarged. As a result, the heart cannot pump enough blood to the rest of the body.
There are many types of cardiomyopathy. Dilated cardiomyopathy is the most common form, but it may be the result of different underlying conditions. Some health care providers use the term to indicate a specific condition, called idiopathic dilated cardiomyopathy. There is no known cause for this type of dilated cardiomyopathy.

Cardiomyopathy, also known as myocardiopathy, is a condition that includes diseases of the heart muscle, resulting in abnormal heart function. It is a progressive impairment of the structure and function of the muscular walls of the heart chambers, and is distinguished from heart muscle impairment caused by hypertension, coronary atherosclerosis, valvular dysfunction, or abnormalities of the pericardium. Cardiomyopathy may be caused by many disorders, or it may be idiopathic (of unknown cause). The main types of cardiomyopathies are dilated, hypertrophic, and restrictive. Cardiomyopathies often cause symptoms of heart failure. Some cardiomyopathies may also cause chest pain, fainting, arrhythmia, or sudden death. Treatment of cardiomyopathies, in addition to lifestyle changes, includes drug therapy with beta-blockers, diuretics, anticoagulants and antiarrhythmics, surgical intervention, pacemaker therapy, and in high-risk patients, implantable cardioverter defibrillator to prevent sudden cardiac death. Cardiac transplantation is an option for patients who do not respond to any of these treatment options.
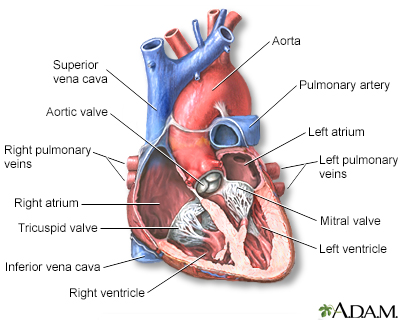
The interior of the heart is composed of valves, chambers, and associated vessels.
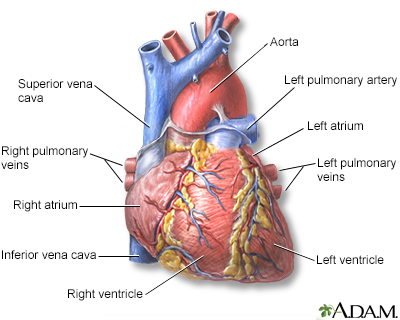
The external structures of the heart include the ventricles, atria, arteries and veins. Arteries carry blood away from the heart while veins carry blood into the heart. The vessels colored blue indicate the transport of blood with relatively low content of oxygen and high content of carbon dioxide. The vessels colored red indicate the transport of blood with relatively high content of oxygen and low content of carbon dioxide.
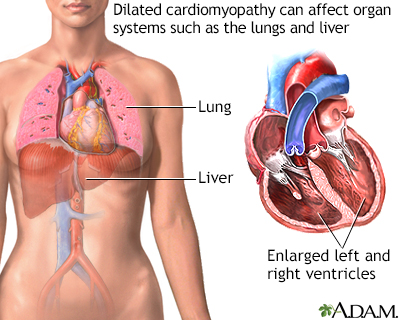
Dilated cardiomyopathy involves enlargement of the heart muscle and is the most common type of cardiomyopathy. The heart muscle is weakened and cannot pump blood efficiently. Decreased heart function affects the lungs, liver, and other body systems.
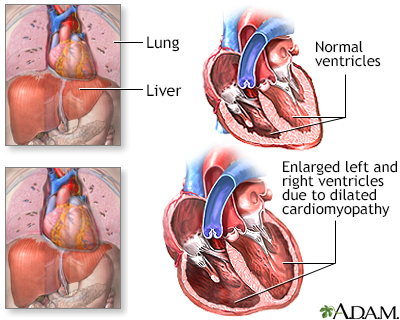
Excessive use of alcohol has a direct toxic effect on the heart muscle cells. The heart muscle becomes weakened and cannot pump blood efficiently. The lack of blood flow affects all parts of the body, resulting in damage to multiple tissues and organ systems. Alcohol may also directly damage the liver.
Causes
The most common causes of dilated cardiomyopathy are:
- Heart disease caused by a narrowing or blockage in the coronary arteries
- Poorly controlled high blood pressure
There are many other causes of dilated cardiomyopathy, including:
- Alcohol or cocaine (or other illegal drug) use (usually heavy use for a prolonged time)
- Diabetes, thyroid disease, or hepatitis
- Medicines that can be toxic to the heart, such as certain medicines used to treat cancer
- Abnormal heart rhythms in which the heart beats very fast for a long period of time
- Autoimmune illnesses
- Conditions that run in families
- Infections that involve the heart muscle
- Heart valves that are either too narrow or too leaky
- During the last month of pregnancy, or within 5 months after the baby is born
- Exposure to heavy metals such as lead, arsenic, cobalt, or mercury
This condition can affect anyone at any age. However, it is most common in adult men.
Symptoms
Symptoms of heart failure are most common. They most often develop slowly over time. However, sometimes symptoms start very suddenly and may be severe.
Common symptoms are:
- Chest pain or pressure (more likely with exercise)
- Cough
- Fatigue, weakness, faintness
- Irregular or rapid pulse
- Loss of appetite
- Shortness of breath with activity or after lying down (or being asleep) for a while
- Swelling of feet and ankles
Cardiomyopathy, also known as myocardiopathy, is a condition that includes diseases of the heart muscle, resulting in abnormal heart function. It is a progressive impairment of the structure and function of the muscular walls of the heart chambers, and is distinguished from heart muscle impairment caused by hypertension, coronary atherosclerosis, valvular dysfunction, or abnormalities of the pericardium. Cardiomyopathy may be caused by many disorders, or it may be idiopathic (of unknown cause). The main types of cardiomyopathies are dilated, hypertrophic, and restrictive. Cardiomyopathies often cause symptoms of heart failure. Some cardiomyopathies may also cause chest pain, fainting, arrhythmia, or sudden death. Treatment of cardiomyopathies, in addition to lifestyle changes, includes drug therapy with beta-blockers, diuretics, anticoagulants and antiarrhythmics, surgical intervention, pacemaker therapy, and in high-risk patients, implantable cardioverter defibrillator to prevent sudden cardiac death. Cardiac transplantation is an option for patients who do not respond to any of these treatment options.
Exams and Tests
During the exam, the provider may find:
- The heart is enlarged.
- Lung crackles (a sign of fluid buildup), heart murmur, or other abnormal sounds.
- The liver is possibly enlarged.
- Neck veins may be bulging.
A number of laboratory tests may be done to determine the cause:
- Antinuclear antibody (ANA), erythrocyte sedimentation rate (ESR), and other tests to diagnose autoimmune illnesses
- Antibody test to identify infections such as Lyme disease and HIV
- Iron tests of the blood
- Serum TSH and T4 test to identify thyroid problems
- Tests for amyloidosis (blood, urine)
Heart enlargement or other problems with the structure and function of the heart (such as weak squeezing) may show up on these tests. They may also help diagnose the exact cause of the problem:
- Echocardiogram (ultrasound of the heart)
- Cardiac stress tests
- Chest x-ray
- Coronary angiogram to look at blood flow through the heart arteries to the heart muscle
- Cardiac catheterization to measure pressures in and around the heart
- CT scan of the heart
- MRI of the heart
- Nuclear heart scan (scintigraphy, MUGA, RNV, PET scan)
Heart biopsy, in which a small piece of heart muscle is removed, may be needed depending on the cause. However, this is rarely done.
Treatment
Things you can do at home to take care of your condition include:
- Know your body, and watch for symptoms that your heart failure is getting worse.
- Watch for changes in your symptoms, heart rate, pulse, blood pressure, and weight.
- Limit how much fluid you drink and how much salt (sodium) you get in your diet (check with your provider about these).
Most people who have heart failure need to take medicines. Some medicines treat your symptoms. Others may help prevent your heart failure from becoming worse, or may prevent other heart problems.
Procedures and surgeries you may need include:
- A pacemaker to help treat slow heart rates or help your heartbeat stay in sync
- A defibrillator that recognizes life-threatening heart rhythms and sends an electrical pulse (shock) to stop them
- Heart bypass (CABG) surgery or angioplasty to improve blood flow to the damaged or weakened heart muscle
- Valve replacement or repair
For advanced cardiomyopathy:
- A heart transplant may be recommended if standard treatments have not worked and heart failure symptoms are very severe.
- Placement of a ventricular assist device or artificial heart may be considered.
Chronic heart failure becomes worse over time. Many people who have heart failure will die from the condition. Thinking about the type of care you may want at the end of life and discussing these issues with loved ones and your health care provider is important.
Outlook (Prognosis)
Heart failure is most often a chronic illness, which may get worse over time. Some people develop severe heart failure, in which medicines, other treatments, and surgery no longer help. Many people are at risk for deadly heart rhythms, and may need medicines or a defibrillator.
When to Contact a Medical Professional
Contact your provider if you have symptoms of cardiomyopathy.
Get emergency medical help right away if you have chest pain, palpitations or fainting.
References
Elliott PM, Olivotto I. Diseases of the myocardium and endocardium. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 47.
Hershberger RE. The dilated, restrictive, and infiltrative cardiomyopathies. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 52.
Mann DL. Management of heart failure patients with reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 50.
Version Info
Last reviewed on: 2/27/2024
Reviewed by: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
