Fibromyalgia
Fibromyositis; FM; Fibrositis
Fibromyalgia is a condition in which a person has long-term pain that is spread throughout their body. The pain is most often accompanied by fatigue, sleep problems, difficulty concentrating, headaches, depression, and anxiety.
People with fibromyalgia may also have tenderness in the joints, muscles, tendons, and other soft tissues.
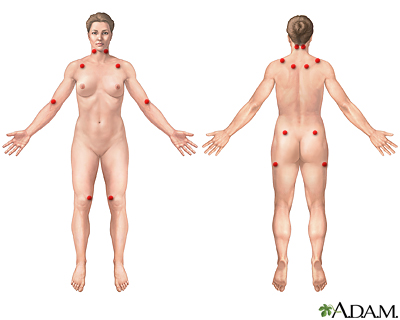
Fibromyalgia is a common rheumatic syndrome indicating widespread pain in fibrous tissues, muscles, tendons, and other connective tissues, resulting in painful muscles without weakness. The cause of this disorder is unknown, although it is a chronic problem that can come and go for years. The nine paired red circles are recognized as common tender points associated with fibromyalgia.
Causes
The cause of fibromyalgia is not known. Researchers think that it is due to a problem with how the central nervous system processes pain signals from nerves. Possible causes or triggers of fibromyalgia include:
- Physical or emotional trauma.
- Abnormal pain response: Areas in the brain that control pain may react differently in people with fibromyalgia.
- Sleep disturbances.
- Infection, such as a virus, although none has been identified.
Fibromyalgia is more common in females as compared to males. Women ages 20 to 50 are the most affected group of people.
The following conditions may be seen with fibromyalgia or have similar symptoms:
- Long-term (chronic) neck or back pain
- Long-term (chronic) fatigue syndrome
- Depression
- Hypothyroidism (underactive thyroid)
- Lyme disease
- Sleep disorders
Symptoms
Widespread pain is the main symptom of fibromyalgia. Fibromyalgia appears to be on one end of a range of chronic widespread pain, which may be present in 10% to 15% of the general population. Fibromyalgia falls on the far end of that pain severity and chronicity scale and occurs in 1% to 5% of the general population.
The central feature of fibromyalgia is chronic pain in multiple sites. These sites are the head, each arm, the chest, the abdomen, each leg, the upper back and spine, and the lower back and spine (including the buttocks).
The pain may be mild to severe.
- It may feel like a deep ache, or a stabbing, burning pain.
- It may feel like it is coming from the joints, although the joints are not affected or damaged and appear normal.
People with fibromyalgia tend to wake up with body pain and stiffness. For some people, pain improves during the day and gets worse at night. Some people have pain all day long.
Pain may get worse with:
- Physical activity
- Cold or damp weather
- Anxiety and stress
Most people with fibromyalgia have at least one of these symptoms: fatigue, depressed mood, or sleep problems. Many people say that they cannot get to sleep or stay asleep, and they feel tired when they wake up (called non-restorative sleep).
Other symptoms in people with fibromyalgia may include:
- Symptoms of irritable bowel syndrome (IBS) or gastroesophageal reflux disease (GERD)
- Memory and concentration problems
- Numbness and tingling in hands and feet
- Reduced ability to exercise
- Tension or migraine headaches
Exams and Tests
To be diagnosed with fibromyalgia, you must have had at least 3 months of widespread pain with one or more of the following:
- Ongoing problems with sleep
- Fatigue
- Thinking or memory problems
It is not necessary for the health care provider to find tender points during a physical exam to make a diagnosis and results of the exam may be normal.
Results from blood and urine tests, and imaging tests are normal. These tests may be done to check for other conditions with similar symptoms. Studies of breathing during sleeping may be done to find out if you have a condition called sleep apnea.
Fibromyalgia is common in every rheumatic disease and may complicate diagnoses and therapy. These disorders include:
- Rheumatoid arthritis
- Osteoarthritis
- Spondyloarthritis
- Systemic lupus erythematosus
Treatment
The goals of treatment are to help relieve pain and other symptoms, to reduce disability, and to help the person cope with the symptoms.
The first type of treatment may involve:
- Physical therapy
- An exercise and fitness program
- Stress-relief methods, including light massage and relaxation techniques
If these treatments do not work, your provider may also prescribe an antidepressant or muscle relaxant. Sometimes, combinations of medicines are helpful.
- The goal of these medicines is to improve your sleep and help you better tolerate pain.
- Medicine should be used along with exercise and behavior therapy.
- Duloxetine (Cymbalta), pregabalin (Lyrica), and milnacipran (Savella) are medicines that are approved by the US Food and Drug Administration (FDA) specifically for treating fibromyalgia.
Other medicines are also used to treat the condition, such as:
- Anti-seizure drugs, such as gabapentin
- Other antidepressants, such as amitriptyline
- Muscle relaxants, such as cyclobenzaprine
- Pain relievers, such as acetaminophen, ibuprofen, naproxen, or tramadol
If you have sleep apnea, a device called continuous positive airway pressure (CPAP) may be prescribed.
Cognitive-behavioral therapy is an important part of treatment. This therapy helps you learn how to:
- Deal with negative thoughts
- Keep a diary of pain and symptoms
- Recognize what makes your symptoms worse
- Seek out enjoyable activities
- Set limits
Complementary and alternative treatments may also be helpful. These may include:
- Tai chi
- Yoga
- Acupuncture
Support groups may also help.
Things you can do to help take care of yourself include:
- Eat a well-balanced diet.
- Avoid caffeine.
- Practice a good sleep routine to improve quality of sleep.
- Exercise regularly. Start with low-level exercise.
There is no evidence that opioids are effective in the treatment of fibromyalgia, and studies have suggested possible adverse effects.
Referral to a clinic with special expertise in diagnosing and treating fibromyalgia may be helpful.
Outlook (Prognosis)
Fibromyalgia is a long-term disorder. Sometimes, the symptoms improve. Other times, the pain may get worse and continue for months or years.
When to Contact a Medical Professional
Contact your provider if you have symptoms of fibromyalgia.
Prevention
There is no known prevention.
References
Borg-Stein J, Brassil ME, Borgstrom HE. Fibromyalgia. In: Frontera WR, Silver JK, Rizzo TD, eds. Essentials of Physical Medicine and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 102.
Clauw DJ. Fibromyalgia. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 253.
Crofford LJ. Fibromyalgia. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 55.
Goldenberg DL. Diagnosing fibromyalgia as a disease, an illness, a state, or a trait? Arthritis Care Res (Hoboken). 2019;71(3):334-336. PMID: 30724034
Lauche R, Cramer H, Häuser W, Dobos G, Langhorst J. A systematic overview of reviews for complementary and alternative therapies in the treatment of the fibromyalgia syndrome. Evid-Based Complement Alternat Med. 2015; 2015:610615. PMID: 26246841
Minhas D, Clauw DJ. Fibromyalgia and related syndromes. In: Hochberg MC, Gravallese EM, Silman AJ, Hejjde D, Weinblatt ME, Weisman MH, eds. Rheumatology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 88.
Version Info
Last reviewed on: 1/25/2023
Reviewed by: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Internal review and update on 07/12/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
