Gastroesophageal reflux in infants
Reflux - infants
Gastroesophageal reflux occurs when stomach contents leak backward from the stomach into the esophagus. This causes "spitting up" in infants.
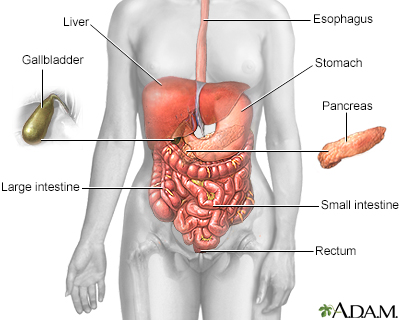
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Causes
When a person eats, food passes from the throat to the stomach through the esophagus. The esophagus is called the food pipe or swallowing tube.
A ring of muscle fibers prevents food at the top of the stomach from moving up into the esophagus. These muscle fibers are called the lower esophageal sphincter, or LES. If this muscle does not close well, food can leak back into the esophagus. This is called gastroesophageal reflux.
A small amount of gastroesophageal reflux is normal in young infants. However, ongoing reflux with frequent vomiting can irritate the esophagus and make the infant fussy. Severe reflux that causes weight loss or breathing problems is not normal.
Do you feel a burning in your chest not long after you eat or lie down? If so, you may have Gastroesophageal reflux disease, or GERD. When we swallow food, it travels down our esophagus into the stomach, where it's greeted by a rush of Hydrochloric acid in the stomach to begin digestion. This acid is so powerful, it could eat the paint right off your car! Fortunately, there's a band of muscle between the stomach and the esophagus - called the Lower Esophageal Sphincter or L-E-S, that clamps down to prevent the stomach contents from moving or refluxing upward and burning the lining of the esophagus. If that band of muscle does not adequately clamp down, this backwash causes the irritation and burning that's known as heartburn or GERD. Maintaining good tight L-E-S muscle tone is the key to preventing this condition. Causes of GERD include being overweight, smoking, and drinking too much alcohol. Certain foods, like chocolate and peppermint and if you're a woman, pregnancy can bring on GERD. To determine if you have GERD, your doctor may request an upper endoscopy exam to look into your esophagus and stomach to diagnose reflux. Other tests can measure the acid and amount of pressure in your esophagus, or if you have blood in your stool. If you do have GERD, lifestyle changes can help. First, avoid foods that cause problems for you and avoid eating large meals. If you're a little on the heavy side, try to lose some weight. Since most GERD symptoms are experienced lying down in bed, let gravity help. Elevating the head of your bed 4 to 6 inches using blocks of wood may help. If symptoms continue, see your doctor or a Gastroenterologist for evaluation and an upper endoscopy exam. Your doctor may suggest you take over-the-counter antacids or may prescribe stronger medications. Call your doctor if you are bleeding, feel like you are choking, have trouble-swallowing, or experience sudden weight loss. The good news is most people who have GERD do not need surgery. For the worst cases, surgeons may perform a laparoscopic procedure to tighten a weak L-E-S muscle. If you have occasional heartburn, antacid tablets can be used as needed. However! If you're having heartburn more than 3 to 4 times a week, see your doctor & take the prescribed medication to prevent this condition.
Symptoms
Symptoms may include:
- Cough, especially after eating
- Excessive crying as if in pain
- Excessive vomiting during the first few weeks of life; worse after eating
- Extremely forceful vomiting
- Not feeding well
- Refusing to eat
- Slow growth
- Weight loss
- Wheezing or other breathing problems
Exams and Tests
The health care provider can often diagnose the problem by asking about the infant's symptoms and doing a physical exam.
Infants who have severe symptoms or are not growing well may need more testing to find the best treatment.
Tests that may be done include:
- Esophageal pH monitoring of stomach contents entering the esophagus
- X-ray of the esophagus
- X-ray of the upper gastrointestinal system after the baby has been given a special liquid, called contrast, to drink
Treatment
Often, no feeding changes are needed for infants who spit up but are growing well and seem otherwise content.
Your provider may suggest simple changes to help the symptoms such as:
- Burp the baby after drinking 1 to 2 ounces (30 to 60 milliliters) of formula, or after feeding on each side if breastfeeding.
- Add 1 tablespoon (2.5 grams) of rice cereal to 2 ounces (60 milliliters) of formula, milk, or expressed breast milk. If needed, change the nipple size or cut a small x in the nipple.
- Hold the baby upright for 20 to 30 minutes after feeding.
- Raise the head of the crib. However, your infant should still sleep on the back, unless your provider suggests otherwise.
When the infant begins to eat solid food, feeding thickened foods may help.
Medicines can be used to reduce acid or increase the movement of the intestines.
Outlook (Prognosis)
Most infants outgrow this condition. Rarely, reflux continues into childhood and causes esophageal damage.
Possible Complications
Complications may include:
- Aspiration pneumonia caused by stomach contents passing into the lungs
- Irritation and swelling of the esophagus
- Scarring and narrowing of the esophagus
When to Contact a Medical Professional
Contact your provider if your baby:
- Is vomiting forcefully and often
- Has other symptoms of reflux
- Has problems breathing after vomiting
- Is refusing food and losing or not gaining weight
- Is crying often
References
Hibs AM. Gastrointestinal reflux and motility in the neonate. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 82.
Khan S, Matta SKR. Gastroesophageal reflux disease. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 349.
Version Info
Last reviewed on: 8/5/2023
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
