Gastrointestinal perforation
Intestinal perforation; Perforation of the intestines; Gastric perforation; Esophageal perforation
A perforation is a hole that develops through the wall of a body organ. This problem may occur in the esophagus, stomach, small intestine, large intestine, rectum, or gallbladder.
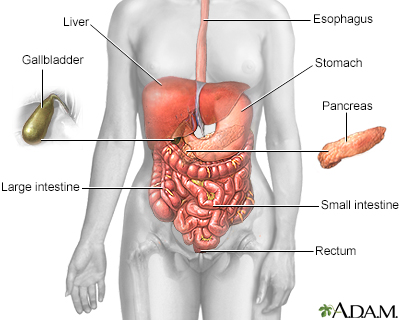
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Causes
Perforation of an organ can be caused by a variety of factors. These include:
- Appendicitis
- Cancer (all types)
- Crohn disease
- Diverticulitis
- Gallbladder disease
- Peptic ulcer disease
- Ulcerative colitis
- Bowel blockage
- Chemotherapy agents
- Increased pressure in the esophagus caused by forceful vomiting
- Ingestion of caustic substances
It may also be caused by surgery in the abdomen or procedures such as colonoscopy or upper endoscopy.
Symptoms
Perforation of the intestine or other organs causes the contents to leak into the abdomen. This causes a severe infection called peritonitis.
Symptoms may include:
- Severe abdominal pain
- Chills
- Fever
- Nausea
- Vomiting
- Shock
Exams and Tests
X-rays of the chest or abdomen may show air in the abdominal cavity. This is called free air. It is a sign of a perforation. If the esophagus is perforated free air can be seen in the mediastinum (around the heart) and in the chest.
A CT scan of the abdomen often shows where the hole is located. The white blood cell count is often higher than normal.
A procedure may help find the area of the perforation, such as an upper endoscopy (EGD) or a colonoscopy.
Treatment
Treatment most often involves emergency surgery to repair the hole.
- Sometimes, a small part of the intestine must be removed. One end of the intestine may be brought out through an opening (stoma) made in the abdominal wall. This is called a colostomy or ileostomy.
- A drain from the abdomen or other organ may also be needed.
In rare cases, people can be treated with antibiotics alone if the perforation has closed. This can be confirmed by a physical exam, blood tests, CT scan, and x-rays.
A perforation from a colonoscopy may sometimes be closed during the procedure without surgery.
Outlook (Prognosis)
Surgery is successful most of the time. However, the outcome will depend on how severe the perforation is, and for how long it was present before treatment. The presence of other illnesses or septic shock can also affect how well a person will do after treatment.
Possible Complications
Even with surgery, infection is the most common complication of the condition. Infections can be either inside the abdomen (abdominal abscess or peritonitis), or throughout the whole body. Body-wide infection is called sepsis. Sepsis can be very serious and can lead to death.
When to Contact a Medical Professional
Contact your health care provider if you have:
- Blood in your stool
- Changes in bowel habits
- Fever
- Nausea
- Severe abdominal pain
- Vomiting
- Call 911 or the local emergency number right away if you or someone else have ingested a caustic substance.
Call the local poison control center emergency number at 1-800-222-1222 if a person has ingested a caustic substance. This hotline number will let you talk to experts in poisoning.
DO NOT wait until the person has symptoms before you call for help.
Prevention
People will often have a few days of pain before the intestinal perforation occurs. If you have pain in the abdomen, see your provider right away. Treatment is much simpler and safer when it is started before the perforation occurs.
References
Brackenridge S, Thompson A. Abdominal sepsis. In: Vincent J-L, Moore FA, Bellomo R, Marini JJ, eds. Textbook of Critical Care. 8th ed. Philadelphia, PA: Elsevier; 2024:chap 90.
Landmann A, Bonds M, Postier R. Acute abdomen. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 46.
Matthews JB, Turaga K. Surgical peritonitis and other diseases of the peritoneum, mesentery, omentum, and diaphragm. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 39.
Version Info
Last reviewed on: 5/14/2024
Reviewed by: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
