Gonococcal arthritis
Disseminated gonococcal infection (DGI); Disseminated gonococcemia; Septic arthritis - gonococcal arthritis
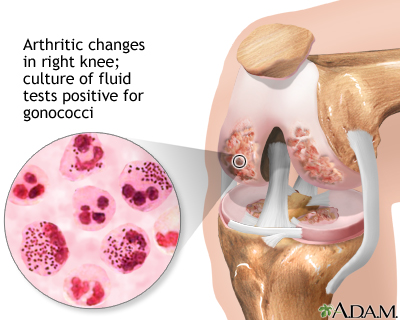
Gonococcal arthritis is inflammation of a joint due to a gonorrhea infection.
Gonococcal arthritis is a type of septic arthritis. This is inflammation of a joint due to a bacterial infection.
Gonoccocal arthritis is an infection, usually of a single joint, that occurs following infection with gonorrhea. If the strain of bacteria is not antibiotic-resistant, recovery is expected.
Causes
Gonococcal arthritis is an infection of a joint. It occurs in people who have gonorrhea, which is caused by the bacteria Neisseria gonorrhoeae. Gonococcal arthritis is a complication of gonorrhea. Gonococcal arthritis affects women more often than men. It is most common among sexually active young adults.
Gonococcal arthritis occurs when the bacteria spread through the blood to a joint. Sometimes, more than one joint is infected.
Symptoms
Symptoms of joint infection may include:
- Fever
- Joint pain for 1 to 4 days
- Pain in the hands or wrists due to tendon inflammation
- Pain or burning during urination
- Single joint pain
- Skin rash (sores are slightly raised, pink to red, and may later contain pus or appear purple)
Exams and Tests
Your health care provider will perform a physical examination and ask about the symptoms.
Tests will be done to check for a gonorrhea infection. This may involve taking samples of tissue, joint fluids, or other body material and sending them to a lab for examination under a microscope. Examples of such tests include:
- Cervical Gram stain
- Culture of joint aspirate
- Joint fluid Gram stain
- Throat culture
- Urine test for gonorrhea
Treatment
The gonorrhea infection must be treated.
There are two aspects of treating a sexually transmitted disease, especially one as easily spread as gonorrhea. The first is to cure the infected person. The second is to locate, test, and treat all sexual contacts of the infected person. This is done to prevent further spread of the disease.
Some locations allow you to take counseling information and treatment to your partner(s) yourself. In other locations, the health department will contact your partner(s).
A treatment routine is recommended by the Centers for Disease Control and Prevention (CDC). Your provider will determine the best and most up-to-date treatment. A follow-up visit 7 days after treatment is important if the infection was complicated, to recheck blood tests and confirm that the infection was cured.
Outlook (Prognosis)
Symptoms usually improve within 1 to 2 days of starting treatment. Full recovery can be expected.
Possible Complications
Untreated, this condition may lead to persistent joint pain.
When to Contact a Medical Professional
Contact your provider if you have symptoms of gonorrhea or gonococcal arthritis.
Prevention
Not having sexual intercourse (abstinence) is the only sure method to prevent gonorrhea. A monogamous sexual relationship with a person who you know does not have any sexually transmitted disease (STD) can reduce your risk. Monogamous means you and your partner do not have sex with any other people.
You can greatly lower your risk for infection with an STD by practicing safer sex. This means using a condom every time you have sex. Condoms are available for both men and women, but they are most commonly worn by the man. A condom must be used properly every time.
Treating all sexual partners is essential to prevent re-infection.
References
Cook PP, Siraj DS. Bacterial arthritis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA , McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116.
Marrazzo JM, Apicella MA. Neisseria gonorrhoeae (gonorrhea). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 212.
Version Info
Last reviewed on: 5/19/2023
Reviewed by: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
