Hyperparathyroidism
Parathyroid-related hypercalcemia; Osteoporosis - hyperparathyroidism; Bone thinning - hyperparathyroidism; Osteopenia - hyperparathyroidism; High calcium level - hyperparathyroidism; Chronic kidney disease - hyperparathyroidism; Kidney failure - hyperparathyroidism; Overactive parathyroid; Vitamin D deficiency - hyperparathyroidism
Hyperparathyroidism is a condition in which 1 or more of the parathyroid glands in your neck produce too much parathyroid hormone (PTH).
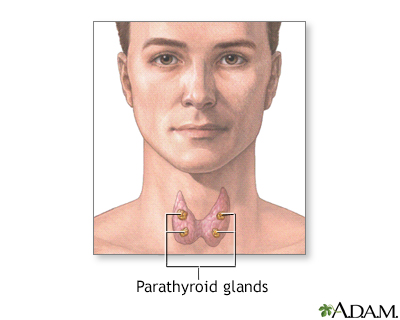
The 4 parathyroid glands are located near or attached to the back side of the thyroid gland and produce parathyroid hormone. Parathyroid hormone regulates calcium, phosphorus, and magnesium balance within the blood and bone by maintaining a balance between the mineral levels in the blood and the bone.
Causes
There are 4 tiny parathyroid glands in the neck, near or attached to the back side of the thyroid gland.
The parathyroid glands help regulate calcium absorption, use and removal by the body. They do this by producing parathyroid hormone (PTH). PTH helps regulate calcium, phosphorus, and vitamin D levels in the blood and bone. It is important for healthy bones.
When the blood calcium level is too low, the body responds by making more PTH. This causes the calcium level in the blood to rise.
If one or more of the parathyroid glands grow larger, it may lead to too much PTH. Most often, the cause is a benign tumor of the parathyroid glands (parathyroid adenoma). These benign tumors are common and happen without a known cause.
- The disease is most common in people over age 60, but it can also occur in younger adults. Hyperparathyroidism in childhood is very unusual.
- Women are more likely to be affected than men.
- Radiation to the head and neck increases the risk.
- Some genetic syndromes (multiple endocrine neoplasia I) make it more likely to have hyperparathyroidism.
- In very rare cases, hyperparathyroidism is caused by parathyroid cancer.
Medical conditions that cause low blood calcium or increased phosphate can also lead to hyperparathyroidism. Common conditions include:
- Conditions that make it hard for the body to remove phosphate
- Kidney damage or failure
- Not enough calcium in the diet
- Too much calcium lost in the urine
- Vitamin D disorders (may occur in children who do not eat a variety of foods, and in older adults who do not get enough sunlight on their skin or who have poor absorption of vitamin D from food such as after bariatric surgery)
- Problems absorbing nutrients from food
Symptoms
Hyperparathyroidism is often diagnosed by common blood tests before symptoms occur.
Symptoms are mostly caused by damage to organs from high calcium level in the blood, or by the loss of calcium from the bones. Symptoms can include:
- Bone pain or tenderness
- Depression and forgetfulness
- Feeling tired, ill, and weak
- Fragile bones of the limbs and spine that can break easily
- Increased amount of urine produced and needing to urinate more often
- Kidney stones
- Nausea and loss of appetite
Exams and Tests
Your health care provider will do a physical exam and ask about symptoms.
Tests that may be done include:
- Creatinine, BUN (kidney function tests)
- PTH blood test
- Calcium blood test
- Alkaline phosphatase
- Magnesium
- Phosphorus
- Vitamin D
- 24-hour urine test - done to determine how much calcium is being filtered out of the body into the urine
Other tests include:
- Bone density exam
- Kidney ultrasound or CT scan (may show kidney stones or calcification)
- Kidney x-rays (may show kidney stones)
- MRI
- Neck ultrasound
- Sestamibi neck scan (to identify the location of the parathyroid adenoma)
Treatment
If you have a mildly increased calcium level and don't have symptoms, you may choose to have regular checkups or get treated.
If you decide to have treatment, it may include:
- Drinking more fluids to prevent kidney stones from forming
- Exercising
- Not taking a type of water pill called thiazide diuretic
- Estrogen for women who have gone through menopause
- Having surgery to remove the overactive glands
If you have symptoms or your blood calcium level is very high, you may need surgery to remove the parathyroid gland that is producing too much PTH.
If you have hyperparathyroidism from a medical condition, your provider may prescribe vitamin D, if you have a low vitamin D level.
If hyperparathyroidism is caused by kidney disease or failure, treatment may include:
- Extra calcium and vitamin D
- Avoiding phosphate in the diet
- The medicine cinacalcet (Sensipar)
- Dialysis or a kidney transplant
- Parathyroid surgery, if the PTH level becomes uncontrollably high
Outlook (Prognosis)
Outlook depends on the cause of hyperparathyroidism.
Possible Complications
Long-term problems that can occur when hyperparathyroidism is not well controlled include:
- Bones become weak, deformed, or can break
- High blood pressure and heart disease
- Kidney stones
- Long-term kidney disease
Parathyroid gland surgery can result in hypoparathyroidism and damage to the nerves that control the vocal cords.
References
Reid LM, Kamani D, Randolph GW. Management of parathyroid disorders. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 123.
Thakker RV. The parathyroid glands, hypercalcemia and hypocalcemia. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 227.
Walker MD, Bilezikian JP. Primary hyperparathyroidism. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 54.
Version Info
Last reviewed on: 5/20/2024
Reviewed by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
