Meconium aspiration syndrome
MAS; Meconium pneumonitis (inflammation of the lungs); Labor - meconium; Delivery - meconium; Neonatal - meconium; Newborn care - meconium
Meconium aspiration syndrome (MAS) refers to breathing problems that a newborn baby may have when:
- There are no other known causes of symptoms
- The baby has passed meconium (stool) into the amniotic fluid during labor or delivery
MAS may occur if the baby breathes (aspirates) this fluid into the lungs.
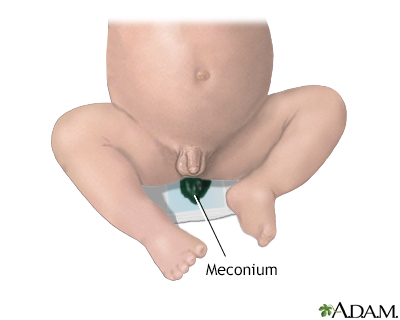
The first bowel movement a baby has is called meconium. Meconium is composed of amniotic fluid, mucus, lanugo (the fine hair that covers the baby's body), bile, and cells that have been shed from the skin and the intestinal tract. Meconium is thick, greenish black, and sticky.
Causes
Meconium is the early stool passed by a newborn soon after birth, before the baby starts to feed and digest milk or formula.
In some cases, the baby passes meconium while still inside the uterus. This can happen when babies are "under stress" due to a decrease in blood and oxygen supply. This is often due to problems with the placenta or the umbilical cord.
Once the baby passes the meconium into the surrounding amniotic fluid, they may breathe it into the lungs. This may happen:
- While the baby is still in the uterus
- During delivery
- Immediately after birth
The meconium can also block the infant's airways right after birth. It can cause breathing problems due to disrupting the balance of proteins normally present as well as causing swelling (inflammation) in the baby's lungs after birth and disrupting the normal changes of blood flow between the heart and lungs following birth.
Risk factors that may cause stress on the baby before birth include:
- "Aging" of the placenta if the pregnancy goes far past the due date
- Decreased oxygen to the infant while in the uterus
- Diabetes in the pregnant mother
- Difficult delivery or long labor
- High blood pressure in the pregnant mother
- Infection in the placenta affecting the baby
Symptoms
Most babies who have passed meconium into the amniotic fluid do not breathe it into their lungs during labor and delivery. They are unlikely to have any symptoms or problems.
Babies who do breathe in this fluid may have the following:
- Bluish skin color (cyanosis) in the infant
- Working hard to breathe (noisy breathing, grunting, using extra muscles to breathe, breathing rapidly)
- No breathing (lack of respiratory effort, or apnea)
- Limpness at birth
Exams and Tests
Before birth, the fetal monitor may show a slow heart rate. During delivery or at birth, meconium can be seen in the amniotic fluid and on the infant.
The infant may need help with breathing or heartbeat right after birth. They may have a low Apgar score.
The health care team will listen to the infant's chest with a stethoscope. This may reveal abnormal breath sounds, especially coarse, crackly sounds.
A blood gas analysis will show:
- Low (acidic) blood pH
- Decreased oxygen
- Increased carbon dioxide
A chest x-ray may show patchy or streaky areas in the infant's lungs.
Treatment
A special care team should be present when the baby is born if traces of meconium are found in the amniotic fluid. This happens in more than 10% of normal pregnancies. If the baby is active and crying, no treatment is needed.
If the baby is not active and crying right after delivery, the team will:
- Warm and maintain normal temperature
- Dry and stimulate the baby
This intervention is often all babies need to begin breathing on their own.
If the baby is not breathing or has a low heart rate:
- The team will help the baby breathe using a face mask attached to a bag that delivers an oxygen mixture to inflate the baby's lungs.
- The infant may be placed in the special care nursery or newborn intensive care unit in order to be watched closely.
Other treatments may include:
- Antibiotics to treat possible infection.
- Breathing machine (ventilator) if baby is unable to breathe on their own or needs a large amount of extra oxygen.
- Oxygen to keep blood levels normal.
- Intravenous (IV) nutrition (nutrition through the veins) if breathing problems are keeping baby from being able to feed by mouth.
- Radiant warmer to maintain body temperature.
- Surfactant to help lungs exchange oxygen. This is only used in more severe cases.
- Nitric oxide (also referred to as NO, an inhaled gas) to help blood flow and oxygen exchange in the lungs. This is only used in severe cases.
- ECMO (extracorporeal membrane oxygenation) is a kind of heart/lung bypass. It may be used in very severe cases.
Outlook (Prognosis)
In most cases of meconium-stained fluid, the outlook is excellent and there are no long-term health effects.
- Only about 5% of babies with meconium-stained fluid will have MAS.
- Babies may need extra support with breathing and nutrition in some cases. This need will often go away in 2 to 4 days. However, rapid breathing may continue for several days.
- MAS rarely leads to permanent lung damage. Some babies with severe MAS may have problems with coughing and wheezing for the first 5 to 10 years.
MAS can occur along with a rare but serious problem with the blood flow to and from the lungs. This is called persistent pulmonary hypertension of the newborn (PPHN).
Prevention
To prevent problems that lead to meconium being present, stay healthy during pregnancy and follow your health care provider's advice.
Your provider will want to be prepared for meconium being present at birth if:
- Your water broke at home and the fluid was clear or stained with a greenish or brown substance.
- Any testing done during your pregnancy indicates there may be problems present.
- Fetal monitoring shows any signs of fetal distress.
References
Ahlfeld SK. Respiratory tract disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 122.
Crowley MA. Spectrum of neonatal respiratory disorders. In: Martin RJ, Fanaroff AA, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 67.
Osman A, Halling C, Crume M, Al Tabosh H, Odackal N, Ball MK. Meconium aspiration syndrome: a comprehensive review. J Perinatol. 2023;43(10):1211-1221. PMID: 37543651
Version Info
Last reviewed on: 12/31/2023
Reviewed by: Mary J. Terrell, MD, IBCLC, Neonatologist, Cape Fear Valley Medical Center, Fayetteville, NC. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
