Nut allergies
Food allergy - nuts; Peanut allergy; Nut allergy
A nut allergy is a type of immune response triggered by tree nuts and peanuts. Peanuts are legumes, not nuts, but many people who are allergic to peanuts are also allergic to nuts. Nut allergies are a type of food allergy.
Most people who develop nut allergies will have them for the rest of their life.
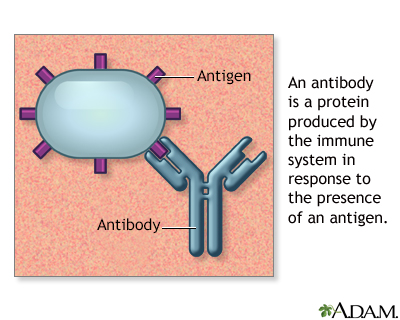
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Causes
The immune system normally protects the body against harmful substances, such as bacteria and viruses. It also reacts to foreign substances called allergens. These are usually harmless, and in most people, do not cause a problem.
If you have a nut allergy, your immune system is overly reactive. When the body identifies a nut allergen, it launches a response. Chemicals such as histamines are released. These chemicals cause allergy symptoms. These symptoms occur every time you come in contact with even a small amount of the nut allergen.
Risk factors for nut and other food allergies include:
- Having eczema as a child
- How early you were exposed to nuts in childhood
Other theories suggest that changes to the microbiome may be a factor. The microbiome is all of the tiny organisms (bacteria, fungi, and others) that normally live on and in our bodies. A number of things may affect the microbiome, including cesarean birth, antibiotic use, and more people living in urban settings. Research is being done to better understand how these things affect the microbiome.
Symptoms
Symptoms usually begin quickly after eating nuts.
Nut allergy symptoms include:
- Hives (urticaria)
- Skin rashes
- Itching of the mouth, throat, eyes, skin, or any other area
- Stomach cramps, diarrhea, nausea, or vomiting
- Stuffy nose, runny nose
- Swelling (angioedema), especially of the eyelids, face, lips, and tongue
- Trouble swallowing or breathing due to swelling in the throat
Nut allergies can cause a life-threatening, whole-body reaction called anaphylaxis. In addition to the above symptoms, you may have low blood pressure and blocked airways. These severe allergy symptoms are a medical emergency.
Exams and Tests
If you suspect that you or your child has a nut allergy, see an allergy specialist doctor (allergist).
Blood or skin tests may be used to confirm that you have an allergy. These tests are:
- Allergy skin test where a small amount of the nut allergen is introduced into the body by pricking the skin.
- Immunoglobulin E (IgE) blood test, which measures levels of IgE in the blood
If results from these tests are unclear, you may have other tests.
A double-blind food challenge is one way to diagnose a nut allergy. During this test, you and your health care provider will not know what you are eating.
With elimination diets, you avoid the suspected food until your symptoms disappear. Then you start eating the foods again to see if you develop an allergic reaction.
In provocation (challenge) testing, you eat a small amount of the suspected food under medical supervision. This type of test may cause severe allergic reactions. Challenge testing should only be done by a trained provider.
Never try to cause a reaction or reintroduce a food on your own. These tests should only be done under the guidance of a provider, especially if your first reaction was severe.
Children 5 years of age and younger with atopic dermatitis should be tested for nut allergies if:
- Dermatitis persists despite treatment
- Allergic symptoms appear right after eating a specific nut
Treatment
Treatment mainly involves:
- Avoiding the nut allergen.
- Knowing what to do in case of accidental exposure.
- Some people may benefit from treatment that helps desensitize them to the allergen.
AVOIDING NUTS
The easiest way to prevent an allergic reaction is to avoid all nuts and peanuts and foods that contain them. Often, nuts and peanuts are processed in the same facility. This increases the risk for cross-contact exposure. Cross-contact is when an allergen is accidentally transferred from one food to another. For example, if you use a knife to spread peanut butter, wipe it off without washing it, and then use it for jelly, the jelly will become contaminated with the proteins from the peanut butter. Even very small amounts of an allergen can cause a reaction.
To avoid consuming nuts you should:
- Read food labels carefully to avoid any foods that contain nuts. These include sweets and baked goods, cereal and granola, whole-grain breads, sauces, soups, and many others.
- Avoid foods with labels that say "may contain traces of" a nut allergen or "produced in a facility" that manufactures nuts or peanuts.
- Always let your restaurant server know that you have a nut allergy. Ask them to make sure there are no nuts or peanuts in your food.
EMERGENCY TREATMENT
There may be a time that you accidentally eat foods with nuts. So you need to know what to do if you are exposed.
Severe allergic reactions (anaphylaxis) need to be treated with a medicine called epinephrine. It can be life-saving when given right away.
Your provider can show you how to use an epinephrine auto-injector such as EpiPen and Auvi-Q. You should have it with you at all times.
If you develop any type of serious or whole-body reaction (even hives) after eating the nut allergen:
- Inject the epinephrine.
- Then call 911 or the local emergency number and follow the instructions you are given, or, go straight to the hospital.
IMMUNOTHERAPY
Oral immunotherapy (desensitization) is a treatment to help you be less sensitive to the nut allergen. This therapy must be done under an allergist's guidance. The allergist will give increasing amounts of the nut allergen (most often peanut powder). This raises the threshold that triggers allergic symptoms. Immunotherapy is not a cure, but it can help reduce the risk of a severe reaction. At the present time, the FDA has only approved oral immunotherapy for peanut allergy.
Support Groups
More information and support for people with nut allergies and their families can be found at:
- American College of Allergy, Asthma and Immunology --
acaai.org/resources/patient-support-organizations/ - Food Allergy Research and Education --
www.foodallergy.org/living-food-allergies/join-community/find-support-group
Outlook (prognosis)
Nut allergies usually last a lifetime. Only about 10% of people will outgrow a tree nut allergy. About 20% of people with peanut allergy will outgrow it.
Possible Complications
Anaphylaxis is a severe, whole-body allergic reaction that is a life-threatening complication.
When to Contact a Medical Professional
Anyone who has had an allergic reaction to any nut should be seen by an allergist.
Steps to take when a nut allergy reaction occurs:
- Call 911 or the local emergency number if you have any serious or whole-body reactions, particularly wheezing or difficulty breathing, after eating any nut.
- If your provider prescribed epinephrine for severe reactions, inject it as soon as possible, even before calling 911. The sooner you inject the epinephrine, the better.
Prevention
Breastfeeding may help prevent allergies from developing in your baby. Otherwise, there is no known way to prevent food allergies.
Avoiding peanuts in early childhood does not appear to prevent, and may even enhance, the development of a peanut allergy. Providers now suggest introducing peanut-containing foods to infants, which may help prevent a peanut allergy. Talk to your child's provider to learn more.
Babies with severe atopic dermatitis can be given peanuts between 4 to 6 months of age to decrease the risk of nut allergies.
References
Albright D, Larkin A, Chong HJ. Allergy and immunology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 4.
Nowak-Wegrzyn A, Burks AW, Sampson HA. Reaction to foods. In: Burks AW, Holgate ST, O’Hehir RE, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 79.
Paller AS, Mancini AJ. Urticarias and other hypersensitivity disorders. In: Paller AS, Mancini AJ, eds. Paller and Mancini -- Hurwitz Clinical Pediatric Dermatology. 6th ed. Philadelphia, PA: Elsevier; 2022:chap 20.
Sicherer SH, Lack G, Jones SM. Food allergy management. In: Burks AW, Holgate ST, O'Hehir RE, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 82.
Version Info
Last reviewed on: 12/24/2023
Reviewed by: Stuart I. Henochowicz, MD, FACP, Clinical Professor of Medicine, Division of Allergy, Immunology, and Rheumatology, Georgetown University Medical School, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
