Occupational asthma
Asthma - occupational exposure; Irritant-induced reactive airways disease
Occupational asthma is a lung disorder in which substances found in the workplace cause the airways of the lungs to swell and narrow. This leads to attacks of wheezing, shortness of breath, chest tightness, and coughing.
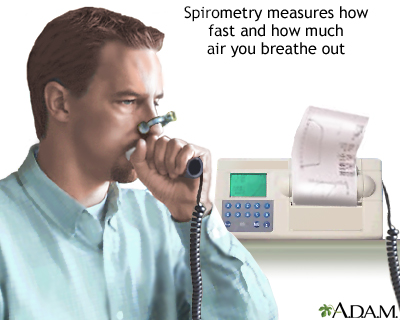
Spirometry is a painless study of air volume and flow rate within the lungs. Spirometry is frequently used to evaluate lung function in people with obstructive or restrictive lung diseases such as asthma or cystic fibrosis.
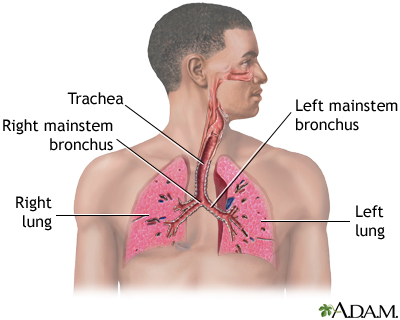
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Causes
Asthma is caused by inflammation (swelling) in the airways of the lungs. When an asthma attack occurs, the lining of the air passages swells and the muscles surrounding the airways activate. This makes the airways narrower and reduces the amount of air that can pass through.
In people who have sensitive airways, asthma symptoms can be triggered by breathing in substances called triggers.
Many substances in the workplace can trigger asthma symptoms, leading to occupational asthma. The most common triggers are wood dust, grain dust, animal dander, fungi, or chemicals.
The following workers are at higher risk:
- Bakers
- Detergent manufacturers
- Drug manufacturers
- Farmers
- Grain elevator workers
- Lab workers (especially those working with laboratory animals)
- Metal workers
- Millers
- Plastics workers
- Woodworkers
Symptoms
Symptoms are usually due to narrowing of the airways and tightening spasms of the muscles lining the airways. This reduces the amount of air that can pass through, which can lead to wheezing sounds.
Symptoms usually occur shortly after you are exposed to the substance. They often improve or go away when you leave work. Some people may not have symptoms until 12 or more hours after being exposed to the trigger.
Symptoms usually get worse toward the end of the work week and may go away on weekends or vacations.
Symptoms include:
- Coughing
- Shortness of breath
- Tight feeling in the chest
- Wheezing
Exams and Tests
Your health care provider will perform a physical exam and ask about your medical history. The provider will listen to your lungs with a stethoscope to check for wheezing.
Tests may be ordered to confirm the diagnosis:
- Blood tests to look for antibodies to the suspected substance
- Bronchial provocation test (test measuring reaction to possible triggers)
- Chest x-ray
- Complete blood count (CBC)
- Lung function tests
- Peak expiratory flow rate, before, during, and after work
Treatment
Avoiding exposure to the substance that is causing your asthma is the best treatment.
Measures may include:
- Changing jobs (though this may be difficult to do)
- Moving to a different location at the work site where there is less exposure to the substance. This may help, but over time, even a very small amount of the substance can trigger an asthma attack.
- Using a respiratory device to eliminate or reduce your exposure may help.
Asthma medicines may help manage your symptoms.
Your provider may prescribe:
- Asthma quick-relief medicines, called bronchodilators, to help relax the muscles of your airways
- Asthma control medicines that are taken every day to prevent symptoms
Outlook (Prognosis)
Occupational asthma may keep getting worse if you continue to be exposed to the substance that is causing the problem, even if medicines improve your symptoms. You may need to change jobs.
Sometimes, symptoms may continue, even when the substance is removed.
In general, the outcome for people with occupational asthma is good. However, symptoms may continue for years after you are no longer exposed in the workplace.
When to Contact a Medical Professional
Contact your provider if you have symptoms of asthma.
Talk to your provider about getting the flu, pneumonia (pneumococcal), COVID-19, and other vaccines.
If you've been diagnosed with asthma, contact your provider right away if you develop a cough, shortness of breath, fever, or other signs of a lung infection, especially if you think you have the flu or COVID-19. Since your lungs are already damaged, it's very important to have the infection treated right away. This will prevent breathing problems from becoming severe, as well as further damage to your lungs.
References
Corry EL, Luong AU, David B. Allergic airway diseases. In: Rich RR, Fleisher TA, Schroeder HW, Weyand CM, Corry DB, Puck JM, eds. Clinical Immunology: Principles and Practice. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 43.
Lemière C, Vandenplas O. Asthma in the workplace. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray & Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 100.
Lemière C, Vandenplas O. Occupational allergy and asthma. In: Burks, AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 56.
Tarlo SM, Redlich CA. Occupational lung disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 81.
Version Info
Last reviewed on: 4/10/2025
Reviewed by: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
