Pancreas divisum
Pancreatic divisum
Pancreas divisum is a birth defect in which parts of the pancreas do not join together. The pancreas is a long, flat organ located between the stomach and spine. It helps in food digestion.
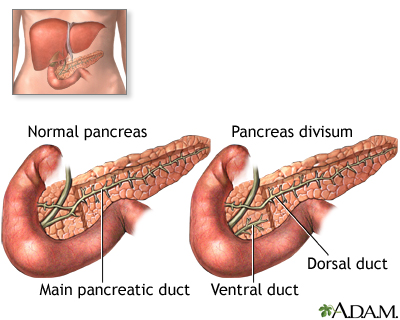
Pancreas divisum is the most common birth defect of the pancreas. The pancreas is an organ that helps in food digestion by producing digestive juices (enzymes) that drain into the intestine through a tube (duct). While the baby is developing inside the uterus, two separate parts of the pancreas come together to form the pancreas and the two ducts join. In pancreas divisum, the two ducts are separate and drainage may be impaired.
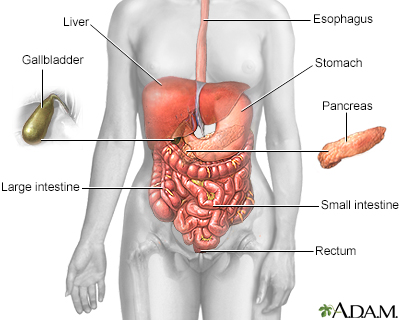
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
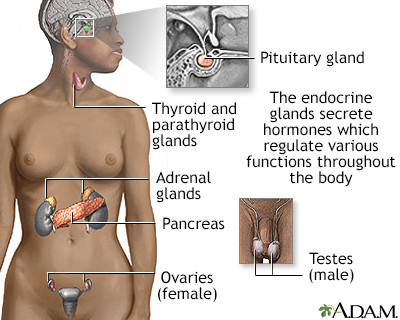
Endocrine glands release hormones (chemical messengers) into the bloodstream to be transported to various organs and tissues throughout the body. For instance, the pancreas secretes insulin, which allows the body to regulate levels of sugar in the blood. The thyroid gets instructions from the pituitary to secrete hormones which determine the rate of metabolism in the body (the more hormone in the bloodstream, the faster the chemical activity; the less hormone, the slower the activity).
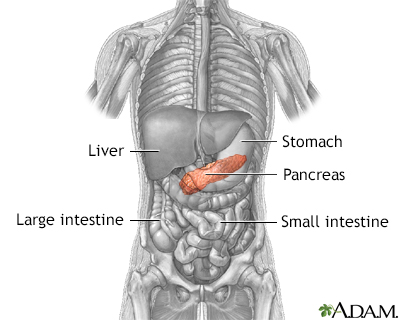
The pancreas is an elongated, tapered gland that is located behind the stomach and secretes digestive enzymes and the hormones insulin and glucagon.
Causes
Pancreas divisum is the most common birth defect of the pancreas. In many cases, this defect goes undetected and causes no problems. The cause of the defect is unknown.
As a baby develops in the womb (uterus), two separate pieces of tissue join together to form the pancreas. Each part has a tube, called a duct. When the parts join together, a final duct, called the pancreatic duct, is formed. Fluid and digestive juices (enzymes) produced by the pancreas normally flow through this duct.
Pancreas divisum occurs if the ducts do not join while the baby develops. Fluid from the two parts of the pancreas drains into separate areas of the upper portion of the small intestine (duodenum). This occurs in 5% to 15% of people.
If a pancreatic duct becomes blocked, swelling and tissue damage (pancreatitis) may develop.
Symptoms
Many people do not have any symptoms. If you have pancreatitis, symptoms include:
- Abdominal pain, most often in the upper abdomen that may be felt in the back
- Abdominal swelling (distention)
- Nausea or vomiting
Exams and Tests
You may have the following tests:
- Abdominal ultrasound
- Abdominal CT scan
- Amylase and lipase blood test
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Magnetic resonance cholangiopancreatography (MRCP)
- Endoscopic ultrasound (EUS)
Treatment
The following treatments may be needed if you have symptoms of the condition, or if pancreatitis keeps returning:
- ERCP with a cut to enlarge the opening where the pancreatic duct drains
- Placement of a stent to prevent the duct from getting blocked
You may need surgery if these treatments do not work.
Outlook (Prognosis)
Most of the time, the outcome is good.
Possible Complications
The main complication of pancreas divisum is pancreatitis.
When to Contact a Medical Professional
Contact your health care provider if you develop symptoms of this disorder.
Prevention
Because this condition is present at birth, there is no known way to prevent it.
References
Adams DB, Coté GA. Pancreas: Pancreas divisum and other variants of dominant dorsal duct anatomy. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:539-650.
Kumar V, Abbas AK, Aster JC, Deyrup AT, Das A, Pancreas. In: Kumar V, Abbas AK, Aster JC, Deyrup AT, Das A, eds. Robbins & Kumar Basic Pathology. 11th ed. Philadelphia, PA: Elsevier; 2023:chap 15.
Mehta MS, Barth BA, Husain SZ. Anatomy, histology, embryology and developmental anomalies of the pancreas. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 55.
Version Info
Last reviewed on: 12/31/2023
Reviewed by: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
