Primary alveolar hypoventilation
Ondine's curse; Ventilatory failure; Diminished hypoxic ventilator drive; Diminished hypercapnic ventilator drive
Alveolar hypoventilation means that a person does not have enough respiratory function to keep the blood level of carbon dioxide in a normal range. Primary means that it is not due to an identifiable cause such as a lung or brain disease. The lungs and airways are normal.
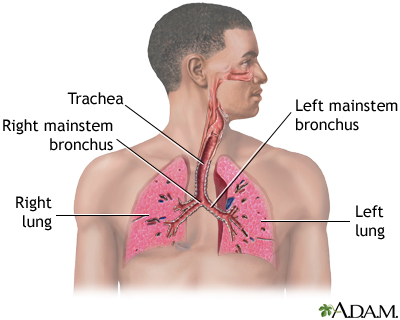
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Causes
Normally, when the oxygen level in the blood is low or the carbon dioxide level is high, there is a signal from the brain to breathe more deeply or quickly. In people with primary alveolar hypoventilation, this change in breathing does not happen.
The cause of this condition is unknown. Some babies have symptoms of this at birth, due to congenital central hypoventilation syndrome. This syndrome is due to a variant in the PHOX2B gene. Children and adults may have a less severe condition that has no definitive cause though some health care providers suspect it may be due to changes in the part of the brain that controls breathing.
Symptoms
Symptoms are usually worse during sleep. Episodes of stopped breathing (apnea) often occur while sleeping. Often there is no shortness of breath during the day.
Symptoms include:
- Bluish coloration of the skin caused by lack of oxygen (cyanosis)
- Daytime drowsiness
- Fatigue
- Morning headaches
- Swelling of the ankles
- Waking up from sleep unrested
- Waking up many times at night
People with this disease may be very sensitive to even small doses of sedatives or narcotics. These medicines can make their breathing problem much worse.
Exams and Tests
Your provider will perform a physical exam and ask about symptoms.
Tests will be done to check for other causes. For example, muscular dystrophy can make the rib muscles weak, and chronic obstructive pulmonary disease (COPD) damages the lung tissue itself. A small stroke can affect the breathing center in the brain.
Tests that may be done include:
- Measuring levels of oxygen and carbon dioxide in the blood (arterial blood gases)
- Chest x-ray or CT scan
- CBC to check oxygen carrying ability of red blood cells
- Lung function tests
- Overnight oxygen level measurements (oximetry)
- Sleep study (polysomnography)
Treatment
Medicines that stimulate the respiratory system may be used but do not always work. Mechanical devices that assist breathing, particularly at night, may be helpful in some people. Oxygen therapy may help in a few people, but may worsen night symptoms in others.
Outlook (Prognosis)
Response to treatment varies.
Possible Complications
Low blood oxygen level can cause high blood pressure in the lung blood vessels. This can lead to cor pulmonale (right-sided heart failure).
When to Contact a Medical Professional
Contact your provider if you have symptoms of this disorder. Seek medical care right away if bluish skin occurs.
Prevention
There is no known prevention. You should avoid using sleep medicines or other medicines that can cause drowsiness.
References
Malhotra A, Powell F. Disorders of ventilatory control. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 74.
Weinberger SE, Cockrill BA, Mandel J. Disorders of ventilatory control. In: Weinberger SE, Cockrill BA, Mandel J, eds. Principles of Pulmonary Medicine. 8th ed. Philadelphia, PA: Elsevier; 2024:chap 18.
Version Info
Last reviewed on: 8/19/2024
Reviewed by: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
