Serum sickness
Drug allergy - serum sickness; Allergic reaction - serum sickness; Allergy - serum sickness
Serum sickness is a reaction that is similar to an allergy. The immune system reacts to medicines that contain proteins used to treat immune conditions. It can also react to antiserum, the liquid part of blood that contains antibodies given to a person to help protect them against germs or poisonous substances.
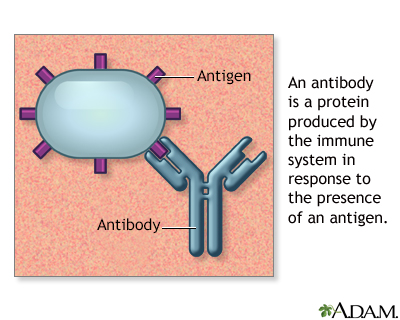
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Causes
Plasma is the clear fluid portion of blood. It does not contain blood cells. But it does contain many proteins, including antibodies, which are formed as part of the immune response to protect against infection.
Antiserum is produced from the plasma of a person or animal that has immunity against an infection or poisonous substance. Antiserum may be used to protect a person who has been exposed to a germ or toxin. For example, you may receive a certain type of antiserum injection:
- If you have been exposed to tetanus or rabies and have never been vaccinated against these germs. This is called passive immunization.
- If you have been bitten by a snake that produces a dangerous toxin.
During serum sickness, the immune system falsely identifies a protein in antiserum as a harmful substance (antigen). The result is an immune system response that attacks the antiserum. Immune system elements and the antiserum combine to form immune complexes, which cause the symptoms of serum sickness.
Certain medicines (such as penicillin, cefaclor, and sulfa) can cause a similar reaction.
Injected proteins such as antithymocyte globulin (used to treat organ transplant rejection) and rituximab (used to treat immune disorders and cancers) can cause serum sickness reactions.
Blood products may also cause serum sickness.
Symptoms
Unlike other medicine allergies, which occur very soon after receiving the medicine, serum sickness develops 7 to 21 days after the first exposure to a medicine. Some people develop symptoms in 1 to 3 days if they have already been exposed to the medicine.
Symptoms of serum sickness can include:
- Fever
- General ill feeling
- Hives
- Itching
- Joint pain and swelling
- Rash
- Swollen lymph nodes
Exams and Tests
The health care provider will perform an exam to look for lymph nodes that are enlarged and tender to the touch.
Tests that may be done include:
- Urine test
- Blood test
Treatment
Medicines, such as corticosteroids, applied to the skin may relieve discomfort from itching and a rash.
Antihistamines may help ease a rash and itching.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, may relieve joint pain. Corticosteroids taken by mouth may be prescribed for severe cases.
The medicine that caused the problem should be stopped. Avoid using that medicine or antiserum in the future.
Outlook (Prognosis)
The symptoms usually go away within a few days.
Possible Complications
If you use the medicine or antiserum that caused serum sickness again in the future, your risk of having another similar reaction is high.
Complications include:
- Inflammation of the blood vessels
- Swelling of the face, arms, and legs (angioedema)
When to Contact a Medical Professional
Contact your provider if you received medicine or antiserum in the last 4 weeks and have symptoms of serum sickness.
Prevention
There is no known way to prevent the development of serum sickness.
People who have had serum sickness or medicine allergy should avoid future use of the antiserum or medicine that caused the reaction.
References
Frank MM, Hester CG. Immune complexes and allergic disease. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 37.
Nowak-Wegrzyn A, Sicherer SH. Serum sickness. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 191.
Version Info
Last reviewed on: 3/31/2024
Reviewed by: Deborah Pedersen, MD, MS, Allergy & Asthma Care, PC, Taunton, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
