Transverse myelitis
TM; Acute transverse myelitis; Secondary transverse myelitis; Idiopathic transverse myelitis
Transverse myelitis is a condition caused by inflammation of the spinal cord. As a result, the covering (myelin sheath) around the nerve cells is damaged. This disturbs the signals between spinal nerves and rest of the body.
Transverse myelitis can cause pain, muscle weakness, paralysis, and bladder or bowel problems.
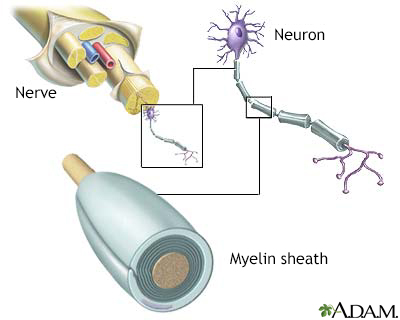
Myelin is the layer that forms around nerve cells. Its purpose is to speed the transmission of impulses along nerve cells.
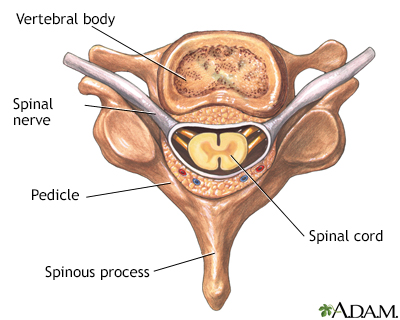
The spinal cord and its peripheral nerves are protected by the vertebral column, a stack of bones which surround and provide support. Between the vertebrae is a fluid-filled disk.
Causes
Transverse myelitis is a rare nervous system disorder. In many cases, the cause is unknown. However, certain conditions may lead to transverse myelitis:
- Bacterial, viral, parasitic, or fungal infection, such as HIV, syphilis, varicella zoster (shingles), West Nile virus, Zika virus, enteroviruses, and Lyme disease
- Immune system disorders, such as multiple sclerosis (MS), Sjögren syndrome, and lupus
- Other inflammatory disorders, such as sarcoidosis, or a connective tissue disease called scleroderma
- Blood vessel disorders that affect the spine
Transverse myelitis affects men and women of all ages and races.
Symptoms
Symptoms of transverse myelitis may develop within a few hours or days. Or, they may develop over 1 to 4 weeks. Symptoms can quickly become severe.
Symptoms tend to occur at or below the damaged area of the spinal cord. Both sides of the body are often affected, but sometimes only one side is affected.
Symptoms include:
Abnormal sensations:
- Numbness
- Pricking
- Tingling
- Coldness
- Burning
- Sensitivity to touch or temperature
Bowel and bladder symptoms:
- Constipation
- Inability to urinate
- Frequent need to urinate
- Difficulty holding urine
- Urine leakage (incontinence)
Pain:
- Sharp or blunt
- May start in your lower back
- May shoot down your arms and legs or wrap around your trunk or chest
Muscle weakness:
- Loss of balance
- Difficulty walking (stumbling or dragging your feet)
- Partial loss of function, which may develop into paralysis
Sexual dysfunction:
- Difficulty having an orgasm (men and women)
- Erectile dysfunction in men
Other symptoms can include loss of appetite, fever, and respiratory problems. Depression and anxiety can occur as a result of dealing with chronic pain and illness.
Exams and Tests
Your health care provider will take your medical history and ask about your symptoms. The provider will also do a nervous system examination to check for:
- Weakness or loss of muscle function, such as muscle tone and reflexes
- Pain level
- Abnormal sensations
Tests to diagnose transverse myelitis and to rule out other causes include:
- MRI of the spinal cord to check for inflammation or abnormalities
- Spinal tap (lumbar puncture)
- Blood tests
Treatment
Treatment for transverse myelitis helps to:
- Treat an infection that caused the condition
- Reduce inflammation of the spinal cord
- Relieve or reduce symptoms
You may be given:
- Steroid medicines through a vein (IV) to decrease inflammation.
- Plasma exchange therapy. This involves removing the liquid part of your blood (plasma) and replacing it with plasma from a healthy donor or with another fluid.
- Medicines to suppress your immune system.
- Medicines to control other symptoms such as pain, spasm, urinary problems, or depression.
Your provider may recommend:
- Physical therapy to help improve muscle strength and balance, and the use of walking aids
- Occupational therapy to help you learn new ways to do daily activities
- Counseling to help you cope with the stress and emotional issues from having transverse myelitis
Support Groups
You can ease the stress of illness by joining a support group. Sharing with others who have common experiences and problems can help you not feel alone.
- National Organization for Rare Disorders (NORD) --
rarediseases.org/rare-diseases/transverse-myelitis/ - Christopher and Dana Reeve Foundation --
www.christopherreeve.org/todays-care/living-with-paralysis/health/causes-of-paralysis/transverse-myelitis/
Outlook (Prognosis)
The outlook for people with transverse myelitis varies. Most recovery occurs within 3 months after the condition occurs. For some, healing may take months to years. About a third of people with transverse myelitis recover completely. Some people recover with moderate disabilities, such as bowel problems and trouble walking. Others have permanent disability and need help with daily activities.
Those who may have poor chance of recovery are:
- People who have rapid onset of symptoms
- People whose symptoms do not improve within the first 3 to 6 months
Transverse myelitis usually only occurs once in most people. It may recur in some people with an underlying cause, such as MS. People who have involvement of only on one side of the spinal cord may be more likely to develop MS in the future.
Possible Complications
Ongoing health problems from transverse myelitis may include:
- Constant pain
- Partial or complete loss of muscle function
- Weakness
- Muscle tightness and spasticity
- Sexual problems
When to Contact a Medical Professional
Contact your provider if:
- You notice a sudden, sharp pain in your back that shoots down your arms or legs or wraps around your trunk
- You develop sudden weakness or numbness of arm or leg
- You have loss of muscle function
- You have bladder problems (frequency or incontinence) or bowel problems (constipation)
- Your symptoms get worse, even with treatment
References
Fabian MT, Krieger SC, Lublin FD. Multiple sclerosis and other inflammatory demyelinating diseases of the central nervous system. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 80.
Lim PAC. Transverse myelitis. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 162.
National Institute of Neurological Disorders and Stroke website. Transverse myelitis.
Perry M, Hemingway C. Demyelinating disorders of the central nervous system. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 640.
Version Info
Last reviewed on: 12/31/2023
Reviewed by: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
