Varicocele
Varicose veins - scrotum
A varicocele is the swelling of the veins inside the scrotum. These veins are found along the cord that holds up a man's testicles (spermatic cord).
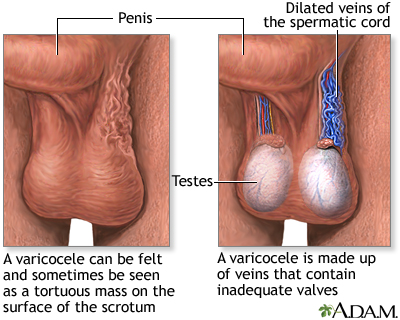
Incompetent or inadequate valves within the veins along the spermatic cord cause a varicocele. The abnormal valves obstruct normal blood flow causing a backup of blood, resulting in enlargement of the veins. Varicoceles usually develop slowly and usually have no symptoms. Varicoceles are a cause of infertility in men.
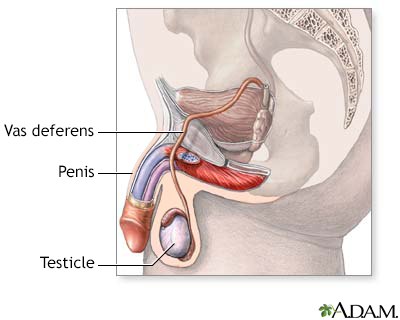
The male reproductive system, viewed from a sagittal section.
Causes
A varicocele forms when valves inside the veins that run along the spermatic cord prevent blood from flowing properly. Blood backs up, leading to swelling and widening of the veins. (This is similar to varicose veins in the legs.)
Most of the time, varicoceles develop slowly. They are more common in men ages 15 to 25 and are most often seen on the left side of the scrotum.
A varicocele in an older man that appears suddenly may be caused by a kidney tumor, which can block blood flow to a vein.
Symptoms
Symptoms include:
- Enlarged, twisted veins in the scrotum
- Dull ache or discomfort
- Painless testicle lump, scrotal swelling, or bulge in the scrotum
- Possible problems with fertility or decreased sperm count
Some men do not have symptoms.
Exams and Tests
You will have an exam of your groin area, including the scrotum and testicles. Your health care provider may feel a twisted growth along the spermatic cord.
Sometimes the growth may not be able to be seen or felt, especially when you are lying down.
The testicle on the side of the varicocele may be smaller than the one on the other side.
You may also have an ultrasound of the scrotum and testicles, as well as an ultrasound of the kidneys.
Treatment
A jock strap or snug underwear may help ease discomfort. You may need other treatment if the pain does not go away or you develop other symptoms.
Surgery to correct a varicocele is called varicocelectomy. For this procedure:
- You will receive some form of anesthesia.
- The urologist (surgeon) will make a cut, most often in the lower abdomen, and tie off the abnormal veins. This directs blood flow in the area to the normal veins. The operation may also be done as a laparoscopic procedure (through small incisions with a camera).
- You will be able to leave the hospital on the same day as your surgery.
- You will need to keep an ice pack on the area for the first 24 hours after surgery to reduce swelling.
An alternative to surgery is varicocele embolization. For this procedure:
- A small hollow tube called a catheter (tube) is placed into a vein in your groin or neck area.
- The provider moves the tube into the varicocele using x-rays as a guide.
- A tiny coil passes through the tube into the varicocele. The coil blocks blood flow to the abnormal vein and sends it to normal veins.
- You will need to keep an ice pack on the area to reduce swelling and wear a scrotal support for a little while.
This method is also done without an overnight hospital stay. It uses a much smaller cut than surgery, so you will heal faster.
Support Groups
Outlook (Prognosis)
A varicocele is often harmless and often does not need to be treated, unless there is a change in the size of your testicle or a problem with fertility.
If you have surgery, your sperm count will likely increase and it may improve your fertility. In most cases, testicular wasting (atrophy) does not improve unless surgery is done early in adolescence.
Possible Complications
Complications from treatment may include:
- Atrophic testis
Blood clot formation- Infection
- Injury to the scrotum or nearby blood vessel
When to Contact a Medical Professional
Contact your provider if you discover a testicle lump or need to treat a diagnosed varicocele.
Prevention
References
Goldstein M. Surgical management of male infertility. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 67.
Palmer LS, Palmer JS. Management of abnormalities of the external genitalia in boys. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 44.
Schlegel PN. Clinical management of male infertility. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 113.
Silay MS, Hoen L, Quadackaers J, et al. Treatment of varicocele in children and adolescents: A systematic review and meta-analysis from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel. Eur Urol. 2019;75(3):448-461. PMID: 30316583
Version Info
Last reviewed on: 7/1/2023
Reviewed by: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
