Viral gastroenteritis (stomach flu)
Rotavirus infection - gastroenteritis; Norwalk virus; Gastroenteritis - viral; Stomach flu; Diarrhea - viral; Loose stools - viral; Upset stomach - viral
Viral gastroenteritis is an infection of the stomach and intestine caused by a virus. The infection can lead to diarrhea and vomiting. It is sometimes called the "stomach flu."
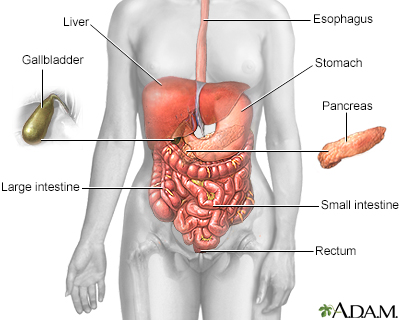
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Causes
Gastroenteritis can affect one person or a group of people who all ate the same food or drank the same water. The germs may get into your system in many ways:
- Directly from food or water
- By way of objects such as plates and eating utensils
- Passed from person to person by way of close contact
Many types of viruses can cause gastroenteritis. The most common viruses are:
- Norovirus (Norwalk-like virus) is common among school-age children. It may also cause outbreaks in hospitals and on cruise ships.
- Rotavirus is the leading cause of gastroenteritis in children. It can also infect adults who are exposed to children with the virus and people living in nursing homes.
- Astrovirus.
- Enteric adenovirus.
- COVID-19 may cause stomach flu symptoms, even when breathing problems are not present.
People with the highest risk for a severe infection include young children, older adults, and people who have a suppressed immune system.
Symptoms
Symptoms most often appear within 4 to 48 hours after contact with the virus. Common symptoms include:
- Abdominal pain
- Diarrhea
- Nausea and vomiting
Other symptoms may include:
- Chills, clammy skin, or sweating
- Fever
- Joint stiffness or muscle pain
- Poor feeding
- Weight loss
Exams and Tests
The health care provider will look for signs of dehydration, including:
- Dry or sticky mouth
- Lethargy or coma (severe dehydration)
- Low blood pressure
- Low or no urine output, concentrated urine that looks dark yellow
- Sunken soft spots (fontanelles) on the top of an infant's head
- No tears
- Sunken eyes
Tests of stool samples may be used to identify the virus that is causing the sickness. Most of the time, this test is not needed. A stool culture may be done to find out if the problem is being caused by bacteria.
Treatment
The goal of treatment is to make sure the body has enough water and fluids. Fluids and electrolytes (salt and minerals) that are lost through diarrhea or vomiting must be replaced by drinking extra fluids. Even if you are able to eat, you should still drink extra fluids between meals.
- Older children and adults can drink sports beverages such as Gatorade, but these should not be used for younger children. Instead, use the electrolyte and fluid replacement solutions or freezer pops available in food and drug stores.
- DO NOT use fruit juice (including apple juice), sodas or cola (flat or bubbly), fruit-flavored gelatin, or broth. These liquids do not replace lost minerals and can make diarrhea worse.
- Drink small amounts of fluid (2 to 4 oz. or 60 to 120 mL) every 30 to 60 minutes. Do not try to force down large amounts of fluid at one time, which can cause vomiting. Use a teaspoon (5 milliliters) or syringe for an infant or small child.
- Babies can continue to drink breast milk or formula along with extra fluids. You do NOT need to switch to a soy formula.
Try eating small amounts of food frequently. Foods to try include:
- Cereals, bread, potatoes, lean meats
- Plain yogurt, bananas, fresh apples
- Vegetables
If you have diarrhea and are unable to drink or keep down fluids because of nausea or vomiting, you may need fluids through a vein (IV). Infants and young children are more likely to need IV fluids.
Parents should closely monitor the number of wet diapers an infant or young child has. Fewer wet diapers is a sign that the infant needs more fluids.
People taking water pills (diuretics) who develop diarrhea may be told by their provider to stop taking them until symptoms improve. However, DO NOT stop taking any prescription medicine without first talking to your provider.
Antibiotics do not work for viruses.
You can buy medicines at the drugstore that can help stop or slow diarrhea.
- Do not use these medicines without talking to your provider if you have bloody diarrhea, a fever, or if the diarrhea is severe.
- Do not give these medicines to children.
Outlook (Prognosis)
For most people, the illness goes away in a few days without treatment.
Possible Complications
Severe dehydration can occur in infants and young children.
When to Contact a Medical Professional
Contact your provider if diarrhea lasts for more than several days or if dehydration occurs. You should also contact your provider if you or your child has these symptoms:
- Blood in the stool
- Confusion
- Dizziness
- Dry mouth
- Feeling faint
- Nausea
- No tears when crying
- No urine for 8 hours or more
- Sunken appearance to the eyes
- Sunken soft spot on an infant's head (fontanelle)
Contact your provider right away if you or your child also have respiratory symptoms, fever or possible exposure to COVID-19.
Prevention
Most viruses and bacteria are passed from person to person by unwashed hands. The best way to prevent stomach flu is to handle food properly and wash your hands thoroughly after using the toilet.
Be sure to observe home isolation and even self-quarantine if COVID-19 is suspected.
A vaccine to prevent rotavirus infection is recommended for infants starting at age 2 months.
References
Bass DM. Rotaviruses, caliciviruses, and astroviruses. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 312.
Fleckenstein JM. Approach to the patient with suspected enteric infection. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 262.
Hammershaimb EA, Kotloff KL. Acute gastroenteritis in children. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 387.
Melia JMP, Sears CL. Infectious enteritis and proctocolitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 110.
Version Info
Last reviewed on: 5/14/2024
Reviewed by: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
