Wilms tumor
Nephroblastoma; Kidney tumor - Wilms
Wilms tumor (WT) is a type of kidney cancer that occurs in children.
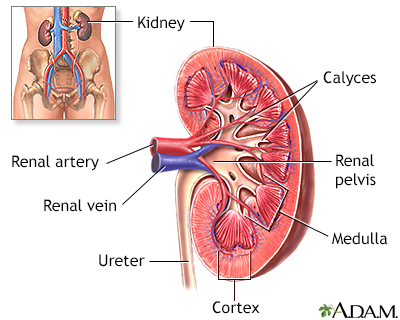
The kidneys are responsible for removing wastes from the body, regulating electrolyte balance and blood pressure, and the stimulation of red blood cell production.
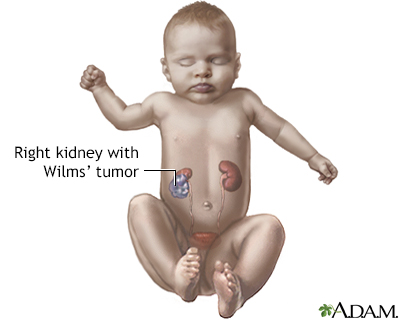
Wilms tumor is a cancerous tumor of the kidney that occurs in children.
Causes
WT is the most common form of childhood kidney cancer. The exact cause of this tumor is unknown in most children.
A missing iris of the eye (aniridia) is a birth defect that is sometimes associated with WT. Other birth defects linked to this type of kidney cancer include certain urinary tract problems and enlargement of one side of the body, a condition called hemihypertrophy.
It is more common among some siblings and twins, which suggests a possible genetic cause.
The disease occurs most often in children about 3 years old. More than 90% of cases are diagnosed before 10 years of age. In rare cases, it is seen in children older than 15 years of age, and in adults.
Symptoms
Symptoms may include any of the following:
- Abdominal pain
- Abnormal urine color
- Constipation
- Fever
- General discomfort or uneasiness (malaise)
- High blood pressure
- Increased growth on only one side of the body
- Loss of appetite
- Nausea and vomiting
- Swelling in the abdomen (abdominal hernia or mass)
- Sweating (at night)
- Blood in urine (hematuria)
Exams and Tests
Your health care provider will perform a physical exam and ask questions about your child's symptoms and medical history. You will be asked if you have a family history of cancer.
A physical exam may show an abdominal mass. High blood pressure may also be present.
Tests include:
- Abdominal ultrasound
- Abdominal x-ray
- BUN
- Chest x-ray or CT scan
- Complete blood count (CBC), may show anemia
- Creatinine (serum and urine)
- Creatinine clearance
- CT scan of the abdomen with contrast
- MRI
- Intravenous pyelogram
- MR angiography (MRA)
- Urinalysis
- Liver function test (transaminases, alkaline phosphatase)
- Calcium
Other tests needed to determine if the tumor has spread may include:
Treatment
If your child is diagnosed with WT, do not prod or push on the child's belly area. Use care during bathing and handling to avoid injury to the tumor site.
The first step in treatment is to stage the tumor. Staging helps the provider determine how far the cancer has spread and to plan for the best treatment. Surgery to remove the tumor is planned as soon as possible. Surrounding tissues and organs may also need to be removed if the tumor has spread.
Radiation therapy and chemotherapy will often be started after surgery, depending on the stage of the tumor.
Chemotherapy given before the surgery is also effective in preventing complications.
Outlook (Prognosis)
Children whose tumor has not spread have a 90% cure rate with appropriate treatment. Prognosis is also better in children younger than 2 years of age.
Possible Complications
The tumor may become quite large, but usually remains self-enclosed. The spread of the tumor to the lungs, lymph nodes, liver, bone, or brain is the most worrisome complication.
High blood pressure and kidney damage may occur as the result of the tumor or its treatment.
Removal of WT from both kidneys may affect kidney function.
Other possible complications of the long-term treatment of WT may include:
- Heart failure
- Secondary cancer elsewhere in the body that develops after the treatment of first cancer
- Short height
When to Contact a Medical Professional
Contact your child's provider if:
- You discover a lump in your child's abdomen, blood in the urine, or other symptoms of WT.
- Your child is being treated for this condition and symptoms get worse or new symptoms develop, mainly cough, chest pain, weight loss, or persistent fevers.
Prevention
For children with a known high risk for WT, screening using ultrasound of the kidneys or prenatal genetic analysis may be suggested.
References
National Cancer Institute website. Wilms tumor and other childhood kidney tumors treatment (PDQ) - health professional version.
Ritchey ML, Cost NG, Shamberger RC. Pediatric urologic oncology: renal and adrenal. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 53.
Weiss RH, Jaimes EA, Hu SL. Kidney cancer. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 41.
Version Info
Last reviewed on: 6/17/2024
Reviewed by: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
