Black widow spider
The black widow spider (Latrodectus genus) has a shiny black body with a red hourglass-shape on its belly area. The venomous bite of a black widow spider is toxic. The genus of spiders, to which the black widow belongs, contains the largest number of venomous species known.
This article is for information only. DO NOT use it to treat or manage a black widow spider bite. If you or someone you are with is bitten, call the local emergency number (such as 911), or the local poison control center can be reached directly by calling the national toll-free Poison Help hotline (1-800-222-1222) from anywhere in the United States.
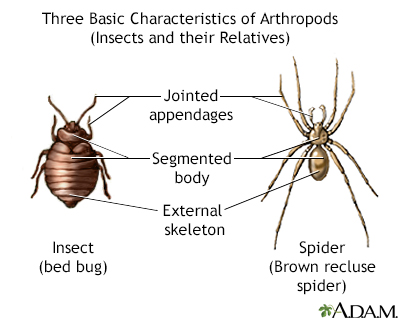
Many arthropods are capable of carrying disease. This illustration shows some of the general characteristics of arthropods.
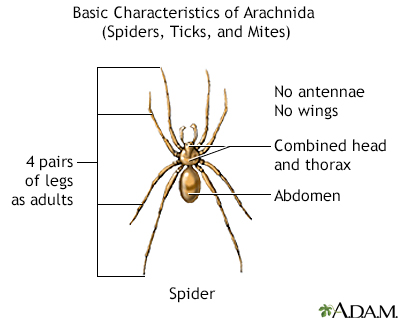
This picture shows the basic features of spiders (arachnids).

This is a black widow spider. Note the red hour glass marking on the abdomen. The bite of the black widow can produce severe symptoms but is seldom fatal, except in young children and older adults. (Image courtesy of the Centers for Disease Control and Prevention.)
Poisonous Ingredient
The venom of the black widow spider contains toxic chemicals, including the neurotoxin alpha latrotoxin, that make people sick.
Where Found
Black widow spiders are found throughout the United States, mostly in the South and West. They are usually found in barns, sheds, stone walls, fences, woodpiles, porch furniture, and other outdoor structures. They are usually, but not always, found near ground level, or within a few feet of the ground. They make irregular, asymmetrical, "disorganized" looking webs.
This genus of spider species is found worldwide. They are most plentiful in temperate and subtropical climates, especially during the summer months, and are common throughout the southern United States.
Wear protective clothing when traveling through areas where these spiders live. DO NOT put your hands or feet in their nests or in their preferred hiding places, such as dark, sheltered areas under logs or underbrush, or other damp, moist areas.
Symptoms
The first symptom of a black widow bite is usually pain similar to a pinprick. This is felt when the bite is made. Some people may not feel it. Minor swelling, redness, and a target-shaped sore may appear.
After 15 minutes to 1 hour, a dull muscle pain spreads from the bite area to the whole body.
- If the bite is on the upper body, you will usually feel most of the pain in your chest.
- If the bite is on your lower body, you will usually feel most of the pain in your abdomen.
The following symptoms can also occur:
- Anxiety
- Difficulty breathing
- Headache
- High blood pressure
- Increased saliva
- Increased sweating
- Light sensitivity
- Muscle weakness
- Nausea and vomiting
- Numbness and tingling around the bite site, then sometimes spreading out from the bite
- Restlessness
- Seizures (usually seen just before death in children who are bitten)
- Very painful muscle cramps or spasms
- Facial swelling in the hours after the bite (This pattern of swelling is sometimes confused with an allergy to the drug used in treatment.)
Pregnant women may have contractions and go into labor.
Home Care
Black widow spider bites are very toxic. Seek medical help right away. Call the Poison Control Center for guidance.
Follow these steps until medical help is given:
- Clean the area with soap and water.
- Wrap ice in a clean cloth and place it on the bite area. Leave it on for 10 minutes and then off for 10 minutes. Repeat this process. If the person has blood flow problems, decrease the time that the ice is on the area to prevent possible skin damage.
- Keep the affected area still, if possible, to prevent the venom from spreading. A homemade splint may be helpful if the bite was on the arms, legs, hands, or feet.
- Loosen clothing and remove rings and other tight jewelry.
Before Calling Emergency
Have this information ready:
- Person's age, weight, and condition
- Time the bite occurred
- Area on the body where the bite occurred
- Type of spider, if possible
Poison Control
Your local poison control center can be reached directly by calling the national toll-free Poison Help hotline (1-800-222-1222) from anywhere in the United States. This national hotline will let you talk to experts in poisoning. They will give you further instructions.
This is a free and confidential service. All local poison control centers in the United States use this national number. You should call if you have any questions about poisoning or poison prevention. It does NOT need to be an emergency. You can call for any reason, 24 hours a day, 7 days a week.
What to Expect at the Emergency Room
If possible, bring the spider to the emergency room. Put it in a secure container.
The health care provider will measure and monitor the person's vital signs, including temperature, pulse, breathing rate, and blood pressure. The person may receive:
- Antivenin, a medicine to reverse the effects of the venom, if available
- Blood and urine tests
- Breathing support, including oxygen, tube through the mouth into the throat, and breathing machine (ventilator)
- Chest x-rays, abdominal x-rays, or both
- ECG (electrocardiogram, or heart tracing)
- Intravenous fluids (IV, or through a vein)
- Medicines to treat symptoms
In general, children, pregnant women, and older people may need to be given Latrodectus antivenin to reverse the effect of the venom. However, it can sometimes cause serious allergic reactions and must be used carefully.
Outlook (Prognosis)
Severe symptoms usually start to improve within 2 to 3 days, but milder symptoms may last for several weeks. Death in a healthy person is very rare. Young children, people who are very ill, and older people may not survive a bite.
References
Boyer LV, Binford GJ, Degan JA. Spider bites. In: Auerbach PS, Cushing TA, Harris NS, eds. Auerbach's Wilderness Medicine. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 43.
Curtis AM, Erickson TB. Venomous animal injuries. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 53.
James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM. Parasitic infestations, stings, and bites. In: James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM, eds. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 20.
Liao L, Norris RL, Nelson EE, Stewart RM. Bites and stings. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 21.
Version Info
Last reviewed on: 7/1/2023
Reviewed by: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
