Cervical cancer - screening and prevention
Cancer cervix - screening; HPV - cervical cancer screening; Dysplasia - cervical cancer screening; Cervical cancer - HPV vaccine
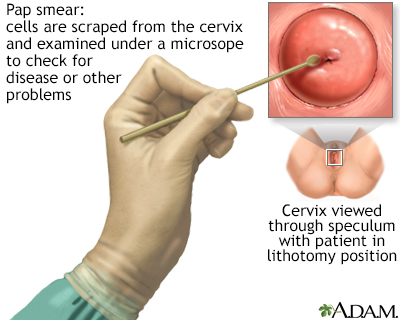
A Pap test is a simple, relatively inexpensive procedure that can easily detect cancerous or precancerous conditions.
Lifestyle and Safer Sex Habits
Almost all cervical cancers are caused by the HPV (human papilloma virus).
- HPV is a common virus that spreads through sexual contact.
- Certain types of HPV are more likely to lead to cervical cancer. These are called high-risk types of HPV.
- Other types of HPV cause genital warts.
HPV can be passed from person to person even when there are no visible warts or other symptoms.
Vaccines to Prevent Cervical Cancer
A vaccine is available to protect against the HPV types that cause most cervical cancer in women. The vaccine is:
- Recommended for girls, boys, women, and men ages 9 through 26. It also may be given to adults ages 27 to 45 if they are at risk for HPV and have not already been vaccinated.
- Given as 2 shots in girls ages 9 through 14, and as 3 shots in teens 15 years or older.
- Best for girls to get by age 11 or before becoming sexually active. However, girls and younger women who are already sexually active can still be protected by the vaccine if they've never been infected.
These safer sex practices can also help reduce your risk of getting HPV and cervical cancer:
- Always use condoms. But be aware that condoms cannot fully protect you. This is because the virus or warts can also be on the nearby skin.
- Have only one sexual partner, whom you know is infection-free.
- Limit the number of sexual partners you have over time.
- Do not get involved with partners who take part in high-risk sexual activities.
- Do not smoke. Cigarette smoking increases the risk of getting cervical cancer.
Pap Smears
Cervical cancer often develops slowly. It starts as precancerous changes called dysplasia. Dysplasia can be detected by a medical test called a Pap smear or Pap test.
Dysplasia is fully treatable. That is why it is important for women to get regular screening tests, so that precancerous cells can be removed before they can become cancer.
At times, the HPV test may be used along with a Pap test. The HPV test can identify the high-risk types of HPV that are known to cause cervical cancer.
Pap test screening should start at age 21. After the first test:
- Women ages 21 through 29 who are at average risk should have a Pap test every 3 years. HPV testing is not recommended for this age group.
- Women ages 30 through 65 have the option to get the HPV test every 5 years with or without a Pap test.
- Women with HIV ages 21 to 29 should have a Pap test every year; after 3 normal tests in a row, test every 3 years.
- Women with HIV ages 30 and older, HPV test with Pap test or just Pap test every year. If screening was normal with Pap test and HPV test, repeat testing every 3 years. If screening was by Pap test only, repeat yearly and after 3 normal tests in a row, every 3 years. Testing should continue throughout your lifetime.
- If you or your sexual partner has other new partners, you should have a Pap test every 3 years.
- Women age over 65 can stop having Pap tests as long as they have had 3 normal tests within the past 10 years and are otherwise not at high risk for cervical cancer.
- Women who have been treated for precancer (cervical dysplasia) should continue to have Pap tests for 20 years after treatment or until age 65, whichever is longer.
- Women who have had a hysterectomy that preserves the cervix (called a supracervical hysterectomy) should continue to have Pap test screening according to the guidelines listed above.
- Women who have had their cervix removed at the time of hysterectomy no longer need Pap tests, unless the hysterectomy was done for cervical cancer or pre-cancer in which cases screening should be continued.
References
American College of Obstetricians and Gynecologists' Committee on Adolescent Health Care, American College of Obstetricians and Gynecologists' Immunization, Infectious Disease, and Public Health Preparedness Expert Work Group. Human Papillomavirus Vaccination: ACOG Committee Opinion, Number 809. Obstet Gynecol. 2020;136(2):e15-e21. PMID: 32732766
Centers for Disease Control and Prevention website. Clinical overview of HPV.
Clinicalinfo.hiv.gov website. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV.
Salcedo MP, Phoolcharoen N, Schmeler KM. Intraepithelial neoplasia of the lower genital tract (cervix, vagina, vulva): etiology, screening, diagnosis, management. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 29.
US Preventive Services Task Force; Curry SJ, Krist AH, Owens DK, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(7):674-686. PMID: 30140884
Version Info
Last reviewed on: 8/23/2023
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 08/15/2024.
