Neck pain or spasms - self care
Pain - neck - self-care; Neck stiffness - self-care; Cervicalgia - self-care; Whiplash - self-care
The pain of whiplash may not appear right away after an accident, but sometimes may take hours to weeks to develop. Symptoms include dizziness, headache, pain or stiffness in the neck, jaw, shoulders, or arms.
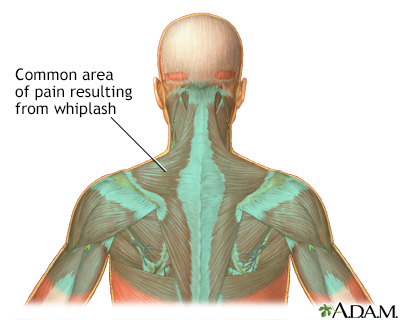
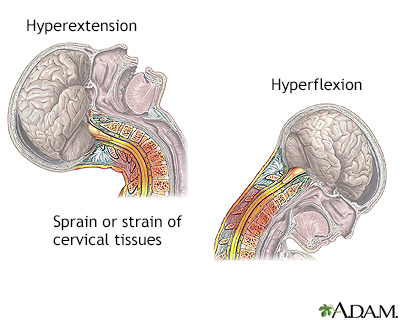
Whiplash is an injury to the soft tissues of the neck. Whiplash injury strains the muscles and ligaments of the neck beyond their normal range of motion. There is often pain and stiffness in the neck for the first few days following a whiplash injury. The pain can also be felt in the surrounding muscle groups in the head, chest, shoulders, and arms.
Pain Relief
You can use one or more of these methods to help reduce neck pain:
- Use over-the-counter pain relievers such as aspirin, ibuprofen (Motrin or Advil), naproxen (Aleve), or acetaminophen (Tylenol).
- Apply heat or ice to the painful area. Use ice for the first 48 to 72 hours, then use heat.
- Apply heat using warm showers, hot compresses, or a heating pad.
- To prevent injuring your skin, do not fall asleep with a heating pad or ice bag in place.
- Have a partner gently massage the sore or painful areas.
- Try sleeping on a firm mattress with a pillow that supports your neck. You may want to get a special neck pillow. You can find them at some pharmacies or retail stores.
Ask your health care provider about using a soft neck collar to relieve discomfort.
- Only use the collar for 2 to 4 days at most.
- Using a collar for longer can make your neck muscles weaker. Take it off from time to time to allow the muscles to get stronger.
Acupuncture also may help relieve neck pain.
Activity Changes
To help relieve neck pain, you may have to reduce your activities. However, providers do not recommend bed rest. You should try to stay as active as you can without making the pain worse.
These tips can help you stay active with neck pain.
- Stop normal physical activity for only the first few days. This helps calm your symptoms and reduce swelling (inflammation) in the area of the pain.
- Do not do activities that involve heavy lifting or twisting of your neck or back for the first 6 weeks after the pain begins.
- If you are unable to move your head around very easily, you may need to avoid driving.
After 2 to 3 weeks, slowly begin to exercise again. Your provider may refer you to a physical therapist. Your physical therapist can teach you which exercises are right for you and when to start.
You may need to stop or ease back on the following exercises during recovery, unless your provider or physical therapist says it is OK:
- Jogging
- Contact sports
- Racquet sports
- Golf
- Dancing
- Weight lifting
- Leg lifts when lying on your stomach
- Sit-ups
Stretches and Exercises
As part of physical therapy, you may receive massage and stretching exercises along with exercises to strengthen your neck. Exercise can help you:
- Improve your posture
- Strengthen your neck and improve flexibility
A complete exercise program should include:
- Stretching and strength training. Follow the instructions of your provider or physical therapist.
- Aerobic exercise. This may involve walking, riding a stationary bicycle, or swimming. These activities can help improve blood flow to your muscles and promote healing. They also strengthen muscles in your stomach, neck, and back.
Stretching and strengthening exercises are important in the long run. Keep in mind that starting these exercises too soon after an injury can make your pain worse. Strengthening the muscles in your upper back can ease the stress on your neck.
Your physical therapist can help you determine when to begin neck stretching and strengthening exercises and how to do them.
Preventing Neck Pain
If you work at a computer or a desk most of the day:
- Stretch your neck every hour or so.
- Use a headset when on the telephone, especially if answering or using the phone is a main part of your job.
- When reading or typing from documents at your desk, place them in a holder at eye level.
- When sitting, make sure that your chair has a straight back with an adjustable seat and back, armrests, and a swivel seat.
Other measures to help prevent neck pain include:
- Avoid standing for long periods. If you must stand for your work, place a stool by your feet. Alternate resting each foot on the stool.
- Do not wear high heels. Wear shoes that have cushioned soles when walking.
- If you drive long-distance, stop and walk around every hour. Do not lift heavy objects just after a long ride.
- Make sure you have a firm mattress and supportive pillow.
- Learn to relax. Try methods such as yoga, tai chi, or massage.
Chronic Neck Pain
For some, neck pain does not go away and becomes a long-lasting (chronic) problem.
Managing chronic pain means finding ways to make your pain tolerable so you can live your life.
Unwanted feelings, such as frustration, resentment, and stress, are often a result of chronic pain. These feelings and emotions can worsen your neck pain.
Ask your provider about prescribing medicines to help you manage your chronic pain. Some with ongoing neck pain take narcotics to control the pain. It is best for you if only one provider is prescribing your narcotic pain medicines.
If you have chronic neck pain, ask your provider about a referral to a:
- Rheumatologist (an expert in arthritis and joint disease)
- Physical medicine and rehabilitation specialist (can help people regain body functions they lost due to medical conditions or injury)
- Neurosurgeon
- Mental health provider
When to Call the Doctor
Contact your provider if:
- Symptoms do not go away in 1 week with self-care
- You have numbness, tingling, or weakness in your arm or hand
- Your neck pain was caused by a fall, blow, or injury, if you cannot move your arm or hand, have someone call 911 or your local emergency number
- The pain gets worse when you lie down or wakes you up at night
- Your pain is so severe that you cannot get comfortable
- You lose control over urination or bowel movements
- You have trouble walking and balancing
References
Bartleson JD. Mechanical and other lesions of the spine, nerve roots, and spinal cord. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 369.
Lemmon R, Leonard J. Neck and back pain. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 31.
Ronthal M. Arm and neck pain. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 32.
Version Info
Last reviewed on: 7/8/2023
Reviewed by: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
