Deciding about an IUD
Contraception - IUD; Birth control - IUD; Intrauterine - deciding; Mirena - deciding; ParaGard - deciding
An intrauterine device (IUD) is a small, plastic, T-shaped device used for birth control. It is inserted into the uterus where it stays to prevent pregnancy.
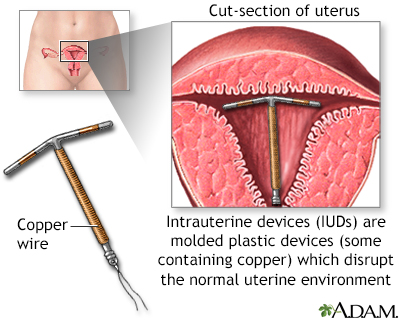
The intrauterine device shown uses copper as the active contraceptive, others use progesterone in a plastic device. IUDs are very effective at preventing pregnancy (less than 2% chance per year for the progesterone IUD, less than 1% chance per year for the copper IUD). IUDs come with increased risk of ectopic pregnancy and perforation of the uterus and do not protect against sexually transmitted disease. IUDs are prescribed and placed by health care providers.
Alternative names
Contraception - IUD; Birth control - IUD; Intrauterine - deciding; Mirena - deciding; ParaGard - deciding
Types of IUDs
You have choices for what type of IUD to have. Talk with your health care provider about which type may be best for you.
Copper-releasing IUDs:
- Start working immediately after being inserted.
- Work by releasing copper ions. These are toxic to sperm. The T-shape also blocks sperm and keeps them from reaching the egg.
- Can stay in the uterus for up to 10 years.
- Can also be used for emergency contraception.
Progestin-releasing IUDs:
- Start to work within 7 days after being inserted.
- Work by releasing progestin. Progestin is a hormone used in many kinds of birth control pills. It prevents the ovaries from releasing an egg.
- Have a T-shape that also blocks the sperm and keeps sperm from reaching an egg.
- Are FDA approved to stay in the uterus for 3 to 8 years. How long depends on the brand. There are 4 brands with different hormone dosages available in the United States: Skyla, Kyleena, Mirena, and Liletta. Mirena can also treat heavy menstrual bleeding and reduce cramps.
How IUDs work
Both types of IUDs prevent sperm from fertilizing an egg.
Progestin-releasing IUDs also work by:
- Making the mucus around the cervix thicker, which makes it harder for sperm get inside the uterus and fertilize an egg
- Thinning the lining of the uterus, which makes it more difficult for a fertilized egg to attach to the uterus
Pros and cons
IUDs have certain benefits.
- They are more than 99% effective at preventing pregnancy.
- You don't need to think about birth control each time you have sex.
- One IUD can last for 3 to 10 years. This makes it one of the cheapest forms of birth control.
- You become fertile again almost immediately after an IUD is removed.
- Copper-releasing IUDs do not have hormonal side effects and may help protect against uterine (endometrial) cancer.
- Both types of IUDs may lower the risk of developing cervical cancer.
There are also downsides.
- IUDs do not prevent sexually transmitted diseases (STDs). To avoid STDs you need to abstain from sex, be in a mutually monogamous relationship, or use condoms.
- A provider needs to insert or remove the IUD.
- While rare, an IUD can slip out of place and need to be removed.
- Copper-releasing IUDs can cause cramps, longer and heavier menstrual periods, and spotting between periods.
- Progestin-releasing IUDs can cause irregular bleeding and spotting during the first few months.
- IUDs may increase the risk for ectopic pregnancy. But women who use IUDs have a very low risk of getting pregnant.
- Some types of IUDs may increase the risk for benign ovarian cysts. But such cysts usually do not cause symptoms and they usually resolve on their own.
IUDs do not appear to increase the risk for pelvic infection. They also do not affect fertility or increase the risk for infertility. Once an IUD is removed, fertility is restored.
Things to think about
You may want to consider an IUD if you:
- Want or need to avoid risks for contraceptive hormones
- Can't take hormonal contraceptives
- Have a heavy menstrual flow and want lighter periods (hormonal IUD only)
You should not consider an IUD if you:
- Are at high risk for STDs
- Have a current or recent history of pelvic infection
- Are pregnant
- Have abnormal Pap tests
- Have cervical or uterine cancer
- Have a very large or very small uterus
References
Isley MM. Postpartum care and long-term health considerations. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 24.
Roe AH, Schreiber CA. Contraception. In: Strauss JF, Barbieri R, Dokras A, Williams CJ, Williams Z, eds. Yen & Jaffe's Reproductive Endocrinology. 9th ed. Philadelphia, PA: Elsevier; 2024:chap 41.
Winikoff B, Grossman D. Contraception. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 220.
Version Info
Last reviewed on: 11/8/2024
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
