External incontinence devices
Condom catheter; Incontinence devices; Fecal collection devices; Urinary incontinence - devices; Fecal incontinence - devices; Stool incontinence - devices
External incontinence devices are products (or appliances). These are worn on the outside of the body. They protect the skin from constant leakage of stool or urine. Certain medical conditions can cause people to lose control of their bowel or bladder.
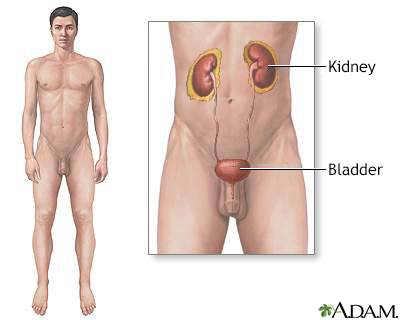
The urinary system is made up of the kidneys, ureters, urethra and bladder.
Information
There are several products available. The features of these different products are listed below.
FECAL INCONTINENCE DEVICES
There are many types of products for managing long-term diarrhea or fecal incontinence. These devices have a drainable pouch attached to an adhesive wafer. This wafer has a hole cut through the center that fits over the anal opening (rectum).
If put on properly, a fecal incontinence device may stay in place for 24 hours. It is important to remove the pouch if any stool has leaked. Liquid stool can irritate the skin.
Always clean the skin and apply a new pouch if any leakage has occurred.
The device should be applied to clean, dry skin:
- Your health care provider may prescribe a protective skin barrier. This barrier is usually a paste. You apply the barrier to the skin before attaching the device. You can put the paste in the skin folds of the buttocks to prevent liquid stool from leaking through this area.
- Spread the buttocks apart, exposing the anus, and apply the wafer and pouch. It may help to have someone help you. The device should cover the skin with no gaps or creases.
- You may need to trim the hair around the anus to help the wafer stick better to the skin.
An enterostomal therapy nurse or skin care nurse can provide you with a list of products that are available in your area.
URINARY INCONTINENCE DEVICES
Urine collection devices are mainly used by men with urinary incontinence. Women are generally treated with medicines and disposable undergarments. An alternative for some women may be a urinary wicking device.
The systems for men most often consist of a pouch or condom-like device. This device is securely placed around the penis. This is often called a condom catheter. A drainage tube is attached at the tip of the device to remove urine. This tube empties into a storage bag, which can be emptied directly into the toilet.
Condom catheters are most effective when applied to a clean, dry penis. You may need to trim the hair around the pubic area for better grip of the device.
You must change the device at least every other day to protect the skin and prevent urinary tract infections. Make sure the condom device fits snugly, but not too tightly. Skin damage may occur if it is too tight.
When you enter a store or restaurant, are you often looking to find the establishments bathroom? If you're having trouble holding in your urine, or if you often leak urine, you probably have what's called urinary incontinence. Normally, the bladder begins to fill with urine from the kidneys. The bladder stretches to allow more and more urine. You should feel the first urge to urinate when there is about 200 mL, just under 1 cup of urine stored in your bladder. A healthy nervous system will respond to this stretching sensation by letting you know that you have to urinate. But, at the same time, the bladder should keep filling. But the system doesn't work correctly in people with urinary incontinence. Some people with urinary incontinence leak urine during activities like coughing, sneezing, laughing, or exercise. This is called stress incontinence. When you have a sudden, strong need to urinate, but can't make it to the bathroom before you do urinate, it's called urge incontinence. Other people have what's called overflow incontinence, when the bladder cannot empty and they dribble. Urinary incontinence can have many causes, and it's most common in older adults. Women are more likely than men to have it. For some people the bladder muscle is overactive. For others, the muscles holding the urine in are weak. And for others, the problem is sensing when the bladder is full. They might have brain or nerve problems, dementia or other health problems that make it hard to feel and respond to the urge to urinate, or problems with the urinary system itself. To treat urinary incontinence, your doctor can help you form a treatment plan. Most likely, exercises to strengthen the muscles of your pelvic floor will be part of that plan. Bladder training exercises can also be effective. And depending on the cause of incontinence, oral medications, or topical estrogen may be helpful. If you have overflow incontinence and cannot empty your bladder completely, you may need to use a catheter. Your doctor can recommend the best catheter for you. For urine leaks, you might wear absorbent pads or undergarments. Whatever else you try, lifestyle changes may help. Aim for an ideal weight. Losing excess weight and increasing exercise both often improve incontinence, especially in women. Also, some specific beverages and foods might increase leaking in some people. For instance, you might try eliminating alcohol, caffeine, carbonated beverages, even decaf coffee. Drink plenty of water, but do NOT drink anything 2 to 4 hours before going to bed. Be sure to empty your bladder before going to bed to help prevent urine leakage at night. Throughout the day, urinate at set times, even if you do not feel the urge. Schedule yourself every 3 to 4 hours. Urinary incontinence is very common, but many people never talk to their doctor about it. Don't let that be you. See your doctor and bring it up at your next doctor's visit.
References
Boone TB, Stewart JN, Martinez LM. Additional therapies for storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 127.
Newman DK, Burgio KL. Conservative management of urinary incontinence: behavioral and pelvic floor therapy, urethral and pelvic devices. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 121.
Version Info
Last reviewed on: 5/17/2024
Reviewed by: Sovrin M. Shah, MD, Associate Professor, Department of Urology, The Icahn School of Medicine at Mount Sinai, New York, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
