Urinary incontinence products
Adult diapers; Disposable urinary collection devices
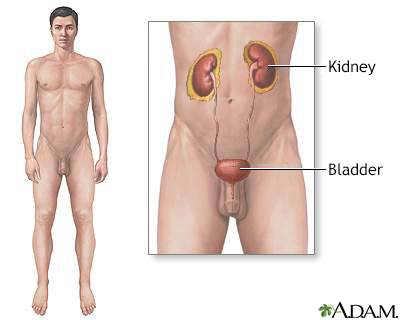
The urinary system is made up of the kidneys, ureters, urethra and bladder.
Information
There are many products to help you manage urinary incontinence. You can decide which product to choose based on:
- How much urine you lose
- Comfort
- Cost
- Durability
- How easy it is to use
- How well it controls odor
- How often you lose urine throughout the day and night
INSERTS AND PADS
You may have tried using sanitary pads to manage urine leaks. However, these products aren't made to absorb urine. So they don't work as well for that purpose.
Pads made for urine leaks can soak up a lot more fluid than sanitary pads. They also have a waterproof backing. These pads are meant to be worn inside your underwear. Some companies make reusable, washable cloth liners or pads that are held in place by waterproof pants.
ADULT DIAPERS AND UNDERWEAR
If you leak a lot of urine, you may need to use adult diapers.
- You can buy either disposable or reusable adult diapers.
- Disposable diapers should fit snugly.
- They usually come in small, medium, large, and extra-large sizes.
- Some diapers have elastic leg seams for a better fit and to prevent leaks.
Reusable underpants may help save money.
- Some types of underwear have a waterproof crotch. They hold a reusable absorbent liner in place.
- Some look like normal underwear, but absorb as well as disposable diapers. Plus you don't need additional pads. They have a special design that quickly pulls fluid away from the skin. They come in different sizes to handle different amounts of leakage.
- Other products include washable, adult cloth diapers or cloth diapers with a plastic cover.
- Some people wear waterproof pants over their underwear for extra protection.
PRODUCTS FOR MEN
- Drip collector -- This is a small pocket of absorbent padding with a waterproof backside. The drip collector is worn over the penis. It is held in place by close-fitting underwear. This works well for men who constantly leak just a little.
- Condom catheter -- You place this product over your penis like you would put on a condom. It has a tube on the end that connects with a collection bag tied to your leg. This device can handle small or large amounts of urine. It has little odor, doesn't irritate your skin, and is easy to use.
- Cunningham clamp -- This device is placed over the penis. This clamp gently keeps the urethra (the tube that carries urine out of the body) closed. You release the clamp when you want to empty your bladder. It can be uncomfortable at first, but most men adjust to it. It is reusable, so it can be less expensive than other options.
PRODUCTS FOR WOMEN
- Pessaries -- These are reusable devices you insert in your vagina to support your bladder and put pressure on your urethra so you don't leak. Pessaries come in different shapes and sizes, such as a ring, cube, or dish. It may take a few tries for your provider to help you find the right fit.
- Urethral insert -- This is a soft plastic balloon that is inserted into your urethra. It works by blocking urine from coming out. You must remove the insert to urinate. Some women use inserts for only part of the day, like when exercising. Others use them throughout the day. To prevent infection, you must use a new sterile insert each time.
- Disposable vaginal insert -- This device is inserted into the vagina like a tampon. It puts pressure on the urethra to prevent leakage. The product is available at drugstores without a prescription.
BED AND CHAIR PROTECTION
- Underpads are flat absorbent pads you can use to protect bed linens and chairs. These underpads, sometimes called Chux, are made of absorbent material with a waterproof backing. They may be disposable or reusable.
- Some new products can pull moisture away from the surface of the pad. This protects your skin from breakdown. Medical supply companies and some larger department stores carry underpads.
- You can also create your own underpads from vinyl tablecloths with flannel backing. Shower curtain liners covered with a flannel sheet also work well. Or, place a rubber pad between layers of bed linens.
KEEP YOUR SKIN DRY
When you use these products, it's important to protect your skin. Skin can break down when in contact with urine for a long time.
- Remove soaked pads right away.
- Remove all wet clothing and linen.
- Thoroughly clean and dry your skin.
- Consider using a skin barrier cream or lotion.
WHERE TO BUY URINARY INCONTINENCE PRODUCTS
You can find most products at your local drugstore, supermarket, or medical supply store. Ask your health care provider for a list of incontinence care products.
The National Association for Continence may be able to help you find products. Call toll-free at 1-800-BLADDER or visit the website:
References
Boone TB, Stewart JN, Martinez LM. Additional therapies for storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 127.
Stiles M, Walsh K. Care of the elderly patient. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 4.
Wagg AS. Urinary incontinence. In: Fillit HM, Rockwood K, Young J, eds. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 8th ed. Philadelphia, PA: Elsevier, 2017:chap 106.
Version Info
Last reviewed on: 7/1/2023
Reviewed by: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
