Gastric bypass surgery
Bariatric surgery - gastric bypass; Roux-en-Y gastric bypass; Gastric bypass - Roux-en-Y; Weight-loss surgery - gastric bypass; Obesity surgery - gastric bypass; Metabolic and bariatric surgery or MBS
Gastric bypass is surgery that helps you lose weight by changing how your stomach and small intestine handle the food you eat.
After the surgery, your stomach will be smaller. You will feel full with less food.
Also, the food you eat will no longer go into some parts of your small intestine that absorb the nutrients in food. Because of this, your body will not get all of the calories from the food you eat.
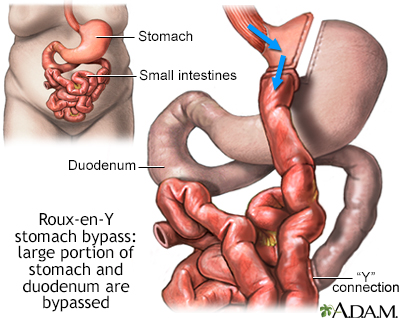
The Roux-en-Y gastric bypass procedure involves creating a stomach pouch out of a small portion of the stomach and attaching it directly to the small intestine, bypassing a large part of the stomach and duodenum. Not only is the stomach pouch too small to hold large amounts of food, but by skipping the duodenum, fat absorption is substantially reduced.
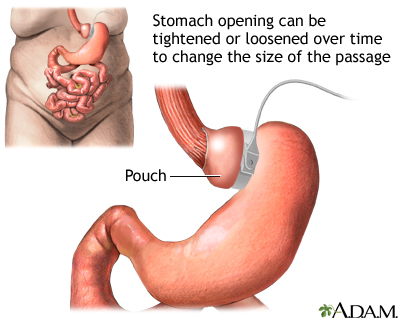
Restrictive gastic operations, such as an adjustable gastric banding procedure, serve only to restrict and decrease food intake and do not interfere with the normal digestive process. In this procedure, a hollow band made of special material is placed around the stomach near its upper end, creating the small pouch and a narrow passage into the larger remaining portion of the stomach. This small passage delays the emptying of food from the pouch and causes a feeling of fullness. The band can be tightened or loosened over time to change the size of the passage. Initially, the pouch holds about 1 ounce of food and later expands to 2-3 ounces.
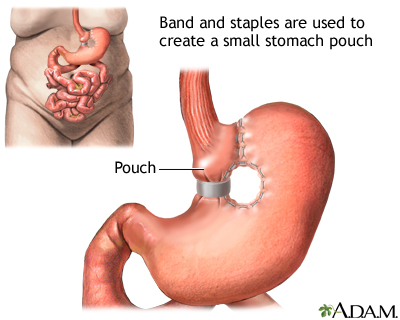
Restrictive gastic operations, such as vertical banded gastroplasty (VGB), serve only to restrict and decrease food intake and do not interfere with the normal digestive process. In this procedure the upper stomach near the esophagus is stapled vertically to create a small pouch along the inner curve of the stomach. The outlet from the pouch to the rest of the stomach is restricted by a band made of special material. The band delays the emptying of food from the pouch, causing a feeling of fullness.
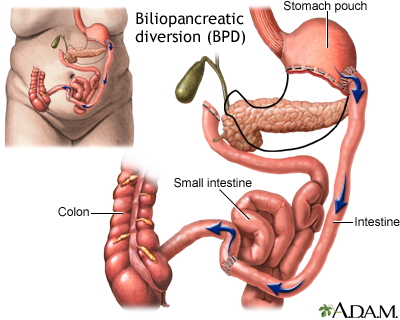
Malabsorptive operations, such as biliopancreatic diversion (BPD), restrict both food intake and the amount of calories and nutrients the body absorbs. In a BPD procedure, portions of the stomach are removed. The small pouch that remains is connected directly to the final segment of the small intestine, completely bypassing the upper part of the intestines. A common channel remains in which bile and pancreatic digestive juices mix prior to entering the colon. Weight loss occurs since most of the calories and nutrients are routed into the colon where they are not absorbed.
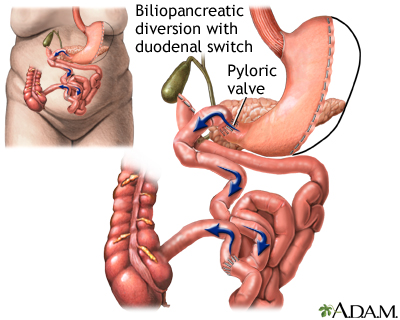
Malabsorptive operations, such as a biliopancreatic diversion with duodenal switch (BPD/DS), restrict both food intake and the amount of calories and nutrients the body absorbs. In this procedure, a larger portion of the stomach is left intact, including the pyloric valve that regulates the release of contents from the stomach into the small intestine. The duodenum is divided near this valve and small intestine divided as well. The portion of the small intestine connected to large intestine is attached to the short duodenal segment next to the stomach. The remaining segment of the duodenum connected to the pancreas and gallbladder is attached to this limb closer to the large instestine. Where contents from these two segments mix is called the common channel, which dumps into the large intestine.
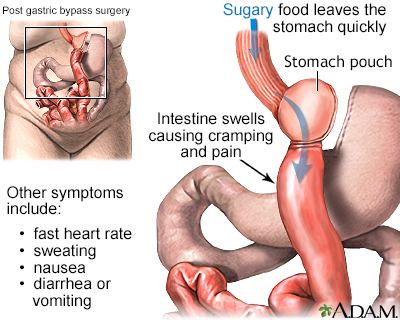
Dumping syndrome occurs when the contents of the stomach empty too quickly into the small intestine. The partially digested food draws excess fluid into the small intestine causing nausea, cramping, diarrhea, sweating, faintness, and palpatations. Dumping usuallly occurs after the consumption of too much simple or refined sugar in people who have had surgery to modify or remove all or part of the stomach.
Description
You will have general anesthesia before this surgery. You will be asleep and pain-free.
There are 2 steps during gastric bypass surgery:
- The first step makes your stomach smaller. Your surgeon uses staples to divide your stomach into a small upper section and a larger bottom section. The top section of your stomach (called the pouch) is where the food you eat will go. The pouch is about the size of a walnut. It holds only about 1 ounce (oz) or 28 grams (g) of food. Because of this you will eat less and lose weight.
- The second step is the bypass. Your surgeon connects a part of your small intestine (the jejunum) to a small hole in your pouch. The food you eat will now travel from the pouch into this new opening and into your small intestine below where it would normally go, thus bypassing part of your small intestine. As a result, your body will absorb fewer calories.
Gastric bypass can be done in two ways. With open surgery, your surgeon makes a large surgical cut to open your belly. The bypass is done by working on your stomach, small intestine, and other organs.
Another way to do this surgery is to use a scope with a tiny camera, called a laparoscope. This camera is placed in your belly. The surgery is called laparoscopy. The scope allows the surgeon to see inside your belly.
In laparoscopic surgery:
- The surgeon makes 4 to 6 small cuts in your belly.
- The scope and instruments needed to perform the surgery are inserted through these cuts.
- The camera is connected to a video monitor in the operating room. This allows the surgeon to view inside your belly while doing the operation.
Advantages of laparoscopy over open surgery include:
- Shorter hospital stay and quicker recovery
- Less pain
- Smaller scars and a lower risk for getting a hernia or infection
This surgery takes about 2 to 4 hours.
Why the Procedure Is Performed
Weight-loss surgery (also called metabolic and bariatric surgery or MBS) may be an option if you have moderate to high-risk obesity and have not been able to lose enough weight through diet, exercise, and medicines.
Health care providers often use the body mass index (BMI) and health conditions such as type 2 diabetes (diabetes that started in adulthood), asthma, and high blood pressure to determine which people are most likely to benefit from MBS.
Gastric bypass surgery is not a quick fix for obesity. It will greatly change your lifestyle. After this surgery, you must eat healthy foods, control portion sizes of what you eat, and exercise. If you do not follow these measures, you may have complications from the surgery, poor weight loss or can even continue to gain weight.
Be sure to discuss the benefits and risks with your surgeon.
This procedure may be recommended if you have:
- A BMI of 35 kilograms/square meter (kg/m2) or more (also called class 2 or class 3 obesity). Someone with a BMI of 35 or more is about 80 or more pounds (lbs) (36.3 kg) over their recommended weight. A normal BMI is 18.5 to 24.9. If you are a member of an Asian population, the BMI threshold for considering surgery is 27.5.
- A BMI of 30 to 34.9 kg/m2 (also called class 1 obesity) and a serious medical condition that might improve with weight loss. Some of these conditions are obstructive sleep apnea, type 2 diabetes, asthma, dyslipidemia, fatty liver disease, nonalcoholic steatohepatitis, and heart disease. If you are a member of an Asian population with one of these conditions, the BMI threshold for considering surgery is 27.5.
Risks
Gastric bypass is major surgery and it has many risks. Some of these risks are very serious. You should discuss these risks with your surgeon.
Risks of having anesthesia and surgery in general include:
- Allergic reactions to medicines
- Breathing problems
- Bleeding, blood clots
- Heart problems
- Infections
Risks of gastric bypass include:
- Gastritis (inflamed stomach lining), heartburn, or stomach ulcers
- Injury to the stomach, intestines, or other organs during surgery
- Leaking from the line where parts of the stomach have been stapled together
- Poor nutrition
- Scarring inside your belly that could lead to a blockage in your bowel in the future
- Vomiting from eating more than your stomach pouch can hold
- Dumping syndrome (when food moves too rapidly from the stomach to the duodenum), especially after eating a meal rich in starches and sugars.
Before the Procedure
Your surgeon will ask you to have tests and visits with other providers before you have this surgery. Some of these are:
- A complete physical exam.
- Blood tests, ultrasound of your gallbladder, and other tests to make sure you are healthy enough to have surgery.
- Visits with your provider to make sure other medical problems you may have, such as diabetes, high blood pressure, and heart or lung problems, are under control.
- Nutritional counseling.
- Classes to help you learn what happens during the surgery, what you should expect afterward, and what risks or problems may occur afterward.
- You may want to visit with a counselor to make sure you are emotionally ready for this surgery. You must be able to make major changes in your lifestyle after surgery.
If you smoke, you should stop several weeks before surgery and not start smoking again after surgery. Smoking slows recovery and increases the risks for problems such as wound infections. Tell your surgeon or provider if you need help quitting.
Tell your surgeon or nurse if:
- You are or could be pregnant
- You are taking any medicines, including medicines, supplements, or herbs you bought without a prescription
During the week before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
Most people stay in the hospital for 1 to 4 days after surgery.
In the hospital:
- You will be asked to sit on the side of the bed and walk a little on the same day you have surgery.
- You may have a tube that goes through your nose into your stomach for 1 or 2 days. This tube helps drain fluids from your intestine.
- You may have a catheter in your bladder to remove urine.
- You will not be able to eat for the first 1 to 3 days. After that, you can have liquids and then pureed or soft foods.
- You may have a tube connected to the larger part of your stomach that was bypassed. The tube will come out of your side and will drain fluids.
- You will wear special stockings on your legs to help prevent blood clots from forming.
- You will receive shots of medicine to prevent blood clots.
- You will receive pain medicine. You will take pills for pain or receive pain medicine through an IV, a catheter that goes into your vein.
You will be able to go home when:
- You can eat liquid or pureed food without vomiting.
- You can move around without a lot of pain.
- You do not need pain medicine through an IV or given by shot.
Be sure to follow instructions for how to care for yourself at home.
Outlook (Prognosis)
Most people lose about 10 to 20 lbs (4.5 to 9 kgs) a month in the first year after surgery. Weight loss will decrease over time. By sticking to your diet and exercise program from the beginning, you will lose more weight.
You may lose one half or more of your extra weight in the first 2 years. You will lose weight quickly after surgery if you are still on a liquid or pureed diet.
Losing enough weight after surgery can improve many medical conditions, including:
- Asthma
- Arthritis
- Heart or cardiovascular disease
- Nonalcoholic fatty liver disease
- Gastroesophageal reflux disease (GERD)
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Some cancers
- Type 2 diabetes
Weighing less should also make it much easier for you to move around and do your everyday activities.
To lose weight and avoid complications from the procedure, you will need to follow the exercise and eating guidelines that your provider and dietitian have given you.
References
Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for metabolic and bariatric surgery. Surg Obes Relat Dis. 2022;18(12):1345-1356. PMID: 36280539
Richards WO, Khaitan L, Torquati A. Morbid obesity. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 48.
Schirmer B. Operations for morbid obesity. In: Yeo CJ, ed. Shackelford's Surgery of the Alimentary Tract. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 63.
Sullivan S, Edmundowicz SA, Morton JM. Surgical and endoscopic treatment of obesity. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 8.
Version Info
Version: 2.0
Last reviewed on: 9/30/2024
Reviewed by: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
