Leg pain
Pain - leg; Aches - leg; Cramps - leg
Leg pain is a common problem. It can be due to a cramp, injury, or other cause.
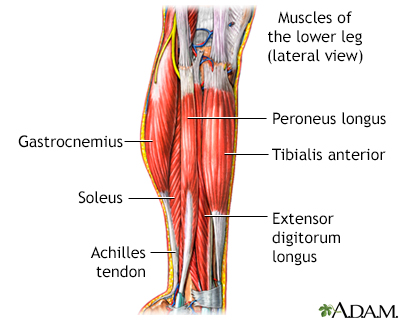
The muscular components of the lower leg include the gastrocnemius, soleus, peroneus longus, tibialis anterior, extensor digitorum longus, and the Achilles tendon.
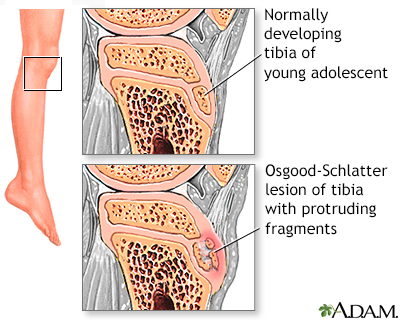
Leg pain in older children or young adolescents can occur for many reasons. An Osgood-Schlatter lesion results from continued trauma to the anterior tibial bone and causes a visible lump below the knee.
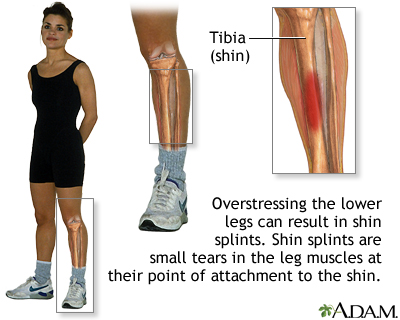
Shin splints is the common name for the medical condition called medial tibial stress syndrome in which pain occurs along the tibia (shin bone) in the front of the lower leg. The pain is a result of small tears in the area the lower leg muscles attachment to the tibia. Shin splints are typically caused from intense or vigorous athletic activity and can be resolved with adequate rest, stretching and modifying your exercise routine.
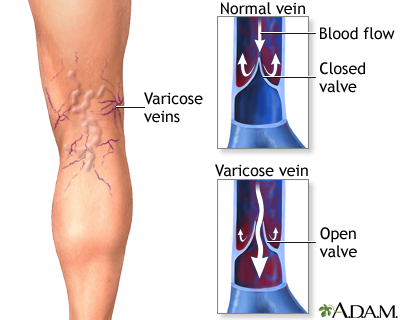
Varicose veins are enlarged, twisted, painful superficial veins resulting from poorly functioning valves. Varicose veins usually occur in the veins of the legs, although it may occur elsewhere. It is a common condition, affecting mostly women.
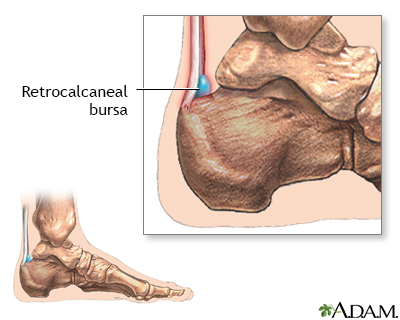
Retrocalcaneal bursitis is an inflammation of the bursa at the back of the heel bone. A bursa is a fluid-filled sac that acts as a cushion and a lubricant between tendons and muscles sliding over bone. Repetitive or over use of the ankle, by doing excessive walking, running, or jumping, can cause this bursa to become irritated and inflamed. Symptoms of bursitis include pain in the heel, especially with walking, running or when the area is touched.
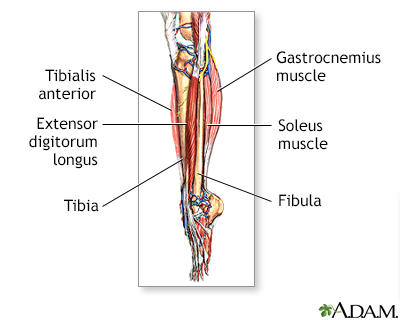
The muscles in the lower leg are divided into several compartments. The muscles in the anterior compartment include the tibialis anterior, extensor halluscis longus, extensor digitorum longus, and peroneous tertius. This group of muscle primarily extends the toes and dorsiflexes the ankle. When there is inflammation in the anterior compartment a painful condition called shinsplints can occur.
Causes
Leg pain can be due to a muscle cramp (also called a charley horse). Common causes of cramps include:
- Dehydration or low amounts of potassium, sodium, calcium, or magnesium in the blood
- Medicines (such as diuretics and statins)
- Muscle fatigue or strain from overuse, too much exercise, or holding a muscle in the same position for a long time
An injury can also cause leg pain from:
- A torn or overstretched muscle (strain)
- Hairline crack in the bone (stress fracture)
- Inflamed tendon (tendinitis)
- Shin splints (pain in the front of the leg from overuse)
Other common causes of leg pain include:
- Peripheral artery disease (PAD), which causes a problem with blood flow in the legs (this type of pain, called claudication, is generally felt when exercising or walking and is relieved by rest)
- Blood clot (deep vein thrombosis), which is sometimes from long-term bed rest but can also occur for no reason
- Infection of the bone (osteomyelitis) or skin and soft tissue (cellulitis)
- Inflammation of the leg joints caused by arthritis or gout
- Nerve damage common to people with diabetes, smokers, and people who consume too much alcohol
- Varicose veins
Less common causes include:
- Cancerous bone tumors (osteosarcoma, Ewing sarcoma, cancer that has spread to the bone from elsewhere in the body)
- Legg-Calve-Perthes disease -- poor blood flow to the hip that may stop or slow the normal growth of the leg
- Noncancerous (benign) tumors or cysts of the femur or tibia (osteoid osteoma)
- Sciatic nerve pain (radiating pain down the leg) caused by a slipped disk in the back
- Slipped capital femoral epiphysis -- most often seen in boys and overweight children age 11 to 15
Home Care
If you have leg pain from cramps or overuse, take these steps first:
- Rest as much as possible.
- Elevate your leg.
- Apply ice for up to 15 minutes. Do this 4 times per day, more often for the first few days.
- Gently stretch and massage cramping muscles.
- Take over-the-counter pain medicines such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin).
Other homecare will depend on the cause of your leg pain.
When to Contact a Medical Professional
Contact your health care provider if:
- Your painful leg is swollen or red.
- You have a fever.
- Your pain gets worse when you walk or exercise and improves with rest.
- Your leg is black and blue.
- Your leg is cold and pale.
- You are taking medicines that may be causing leg pain. DO NOT stop taking or change any of your medicines without talking to your provider.
- Self-care steps do not help.
What to Expect at Your Office Visit
Your provider will perform a physical exam and look at your legs, feet, thighs, hips, back, knees, and ankles.
Your provider may ask questions such as:
- Where on the leg is the pain? Is the pain in one or both legs?
- Is the pain dull and aching or sharp and stabbing? Is the pain severe? Is the pain worse at any time of day?
- What makes the pain feel worse? Does anything make your pain feel better?
- Do you have any other symptoms such as numbness, tingling, back pain, or fever?
Your provider may recommend tests or physical therapy for some causes of leg pain.
References
Anthony KK, Schanberg LE. Musculoskeletal pain syndromes. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 193.
Hogrefe C, Terry M. Leg pain and exertional compartment syndromes. In: Miller MD, Thompson SR. eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 113.
Silverstein JA, Moeller JL, Hutchinson MR. Common issues in orthopedics. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier; 2016:chap 30.
Smith G, Shy ME. Peripheral neuropathies. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 388.
Weitz JI, Eikelboom JW. Venous thrombosis and embolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 68.
White CJ. Atherosclerotic peripheral arterial disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 65.
Version Info
Last reviewed on: 7/8/2023
Reviewed by: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
