Scales
Skin flaking; Scaly skin; Papulosquamous disorders; Ichthyosis
Scales are a visible peeling or flaking of outer skin layers. These layers are called the stratum corneum.
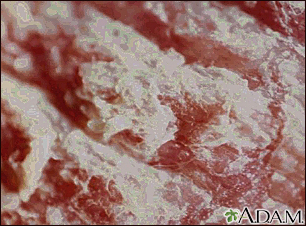
This picture shows a 400% magnification of psoriasis. The whitish scales give the silvery appearance to the typical psoriasis lesion.

This is a picture of Athlete's foot (tinea pedis). Tinea infection is caused by a fungus that grows on the skin, and is also referred to as ringworm. Cutaneous (skin) tinea infections are often named by their location such as pedis, meaning foot.

This view shows the red, scaly patches called plaques that are characteristic of atopic dermatitis.

This is a picture of ringworm, tinea manum, on the finger. This fungal infection is inflamed and scaly.
Causes
Scales may be caused by dry skin, certain inflammatory skin conditions, or infections.
Examples of disorders that can cause scales include:
- Eczema
- Fungal infections such as ringworm or tinea versicolor
- Psoriasis
- Seborrheic dermatitis
- Pityriasis rosea
- Discoid lupus erythematosus, an autoimmune disorder
- Genetic skin disorders called ichthyoses
Home Care
If your health care provider diagnoses you with dry skin, you'll likely be recommended the following self-care measures:
- Moisturize your skin with an ointment, cream, or lotion 2 to 3 times a day, or as often as needed.
- Moisturizers help lock in moisture, so they work best on damp skin. After you bathe, pat your skin dry then apply your moisturizer.
- Bathe only once a day. Take short, warm baths or showers. Limit your time to 5 to 10 minutes. Avoid taking hot baths or showers.
- Instead of regular soap, try using gentle skin cleansers or soap with added moisturizers.
- Avoid scrubbing your skin.
- Drink plenty of water.
- Try over-the-counter cortisone creams or lotions if your skin is inflamed.
If your provider diagnoses you with a skin disorder, such as an inflammatory or fungal disease, follow instructions on home care. This may include using a medicine on your skin. You may also need to take a medicine by mouth.
When to Contact a Medical Professional
Call your provider if your skin symptoms continue and self-care measures aren't helping.
What to Expect at Your Office Visit
Your provider will perform a physical exam to look closely at your skin. You may be asked questions such as when the scaling began, what other symptoms you have, and any self-care you've done at home.
You may need blood tests to check for other conditions.
Treatment depends on the cause of your skin problem. You may need to apply medicine to the skin, or take medicine by mouth.
References
Dinulos JGH. Psoriasis and other papulosquamous diseases. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 8.
Marks JG, Miller JJ. Scaling papules, plaques, and patches. In: Marks JG, Miller JJ, eds. Lookingbill and Marks' Principles of Dermatology. 6th ed. Philadelphia, PA: Elsevier; 2019:chap 9.
Version Info
Last reviewed on: 6/7/2023
Reviewed by: Elika Hoss, MD, Assistant Professor of Dermatology, Mayo Clinic, Scottsdale, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
