Uroflowmetry
Uroflow
Uroflowmetry is a test that measures the volume of urine released from the body, the speed with which it is released, and how long the release takes.
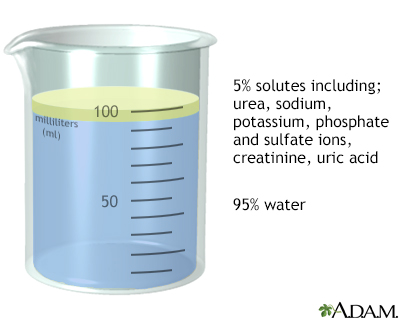
Urine is the liquid waste product excreted by the kidneys. It is stored in the bladder until it is emptied out through the urethra.
How the Test is Performed
You will urinate into a urinal or toilet fitted with a machine that has a measuring device.
You will be asked to begin urinating after the machine has started. When you finish, the machine will make a report for your health care provider.
How to Prepare for the Test
Your provider may ask you to temporarily stop taking medicines that can affect the test results.
Uroflowmetry is best done when you have a full bladder. Do not urinate for at least 2 hours before the test. Drink extra fluids so you will have plenty of urine for the test. The test is the most accurate if you urinate at least 5 ounces (150 milliliters) or more.
Do not place any toilet tissue in the test machine.
How the Test will Feel
The test involves normal urination, so you should not experience any discomfort.
Why the Test is Performed
This test is useful in evaluating the function of the urinary tract. In most cases, a person having this test will report urination that is too slow.
Normal Results
Normal values vary depending on age and sex. In men, urine flow declines with age. Women have less change with age.
What Abnormal Results Mean
Results are compared with your symptoms and physical exam. A result that may need treatment in one person may not need treatment in another person.
Several circular muscles around the urethra normally regulate urine flow. If any of these muscles becomes weak or stops working, you may have an increase in urine flow or urinary incontinence.
If there is a bladder outlet obstruction or if the bladder muscle is weak, you may have a decrease in urine flow. The amount of urine that remains in your bladder after urinating can be measured with ultrasound.
Your provider should explain and discuss any abnormal results with you.
Risks
There are no risks with this test.
References
Brucker BM, Nitti VW. Urodynamic and video-urodynamic evaluation of the lower urinary tract. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 114.
Capogrosso P, Salonia A, Montorsi F. Evaluation and nonsurgical management of benign prostatic hyperplasia. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 145.
Rosenman AE. Pelvic floor disorders: pelvic organ prolapse, urinary incontinence, and pelvic floor pain syndromes. In: Hacker NF, Gambone JC, Hobel CJ, eds. Hacker & Moore's Essentials of Obstetrics and Gynecology. 6th ed. Philadelphia, PA: Elsevier; 2016:chap 23.
Version Info
Last reviewed on: 1/1/2025
Reviewed by: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
