Preschoolers From Low-Income Families May Have Worse Health and Benefit Less From Health Promotion Interventions Than Children With Higher Socioeconomic Status
Mount Sinai study focused on Harlem preschools emphasizes the need for specialized health promotion programs in classrooms starting at an early age
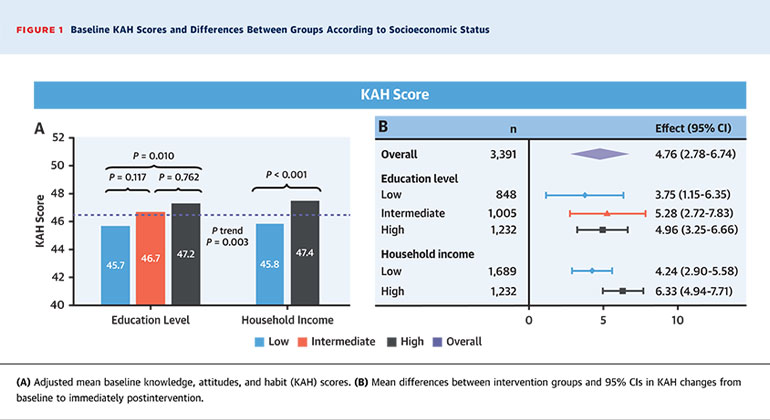
Figure: Baseline KAH Scores and Differences Between Groups According to Socioeconomic Status
Low socioeconomic status can negatively impact children’s health in preschool, along with their ability to follow specialized health education intervention programs, Mount Sinai researchers found in an international study focused on health promotion in schools, including those in the Harlem section of New York City. The results, published September 18 in the Journal of American College of Cardiology, stress the importance of introducing a specialized health curriculum in classrooms starting in preschool.
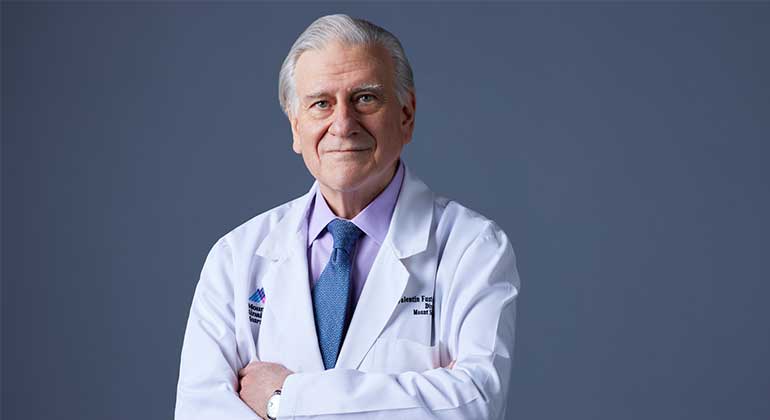
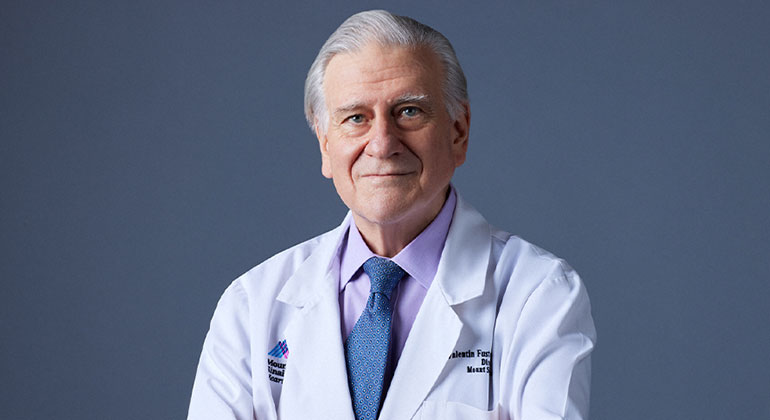
“This study shows that socioeconomic factors, including lower household income and education level, can negatively impact children’s health starting in preschool and emphasizes the importance of promoting healthy lifestyle habits through a specialized school curriculum focused on nutrition and exercise starting in preschool to prevent cardiovascular disease later in life. It is also important to not just educate children, but also teach their caretakers and teachers about healthy habits to further support these efforts,” says Valentin Fuster, MD, PhD, President of Mount Sinai Heart, Physician-in-Chief of The Mount Sinai Hospital, and General Director of the Spanish National Center for Cardiovascular Research (CNIC). Dr. Fuster created and led the trial, known as the FAMILIA Project at Mount Sinai Heart.
The study is part of an ambitious multinational effort to intervene early in the lives of children, their caretakers, and teachers so they can form a lifetime of heart-healthy habits. Researchers conducted the work in 15 Head Start Schools in Harlem, a socioeconomically disadvantaged area that is commonly linked to higher rates of obesity, heart disease, and other health issues. The work was also done in schools in Madrid, Spain (middle to high economic status), and Bogotá, Colombia (middle to low economic status).
Researchers analyzed a total of 3,839 children between three and five years old—562 students in Harlem, 1,216 in Bogotá, and 2,061 in Madrid. At the beginning, children had their weight and height measured and answered a simple guided questionnaire, which included pictures for easier comprehension, to test their knowledge, attitudes, and behaviors regarding diet, physical activity, how the human body and heart works, and emotions.
Children in half of the preschools (the control group) had their regular classroom curriculum, while children in the other preschools (the intervention group) went through a different learning program created by cardiologists, psychologists, and educators over a four-month period. In this program, students had specialized classwork, where teachers taught them about healthy diet, physical activity, how the human body works, and managing emotions. Caregivers were also told to engage in specific activities with their children on weekends during the four months, including buying fresh fruit at the grocery store and choosing physical activity over sedentary behavior. After four months, researchers reassessed children’s weight and height and gave that same questionnaire to children in both the control and intervention groups and compared them.
In this study, researchers specifically looked at household income and educational level, and how they impact students’ knowledge, attitudes, and habits (KAH) toward a healthy lifestyle, and their body mass index z-scores (zBMI). They assessed how socioeconomic status impacted children’s health before and after intervention.
The overall adjusted baseline KAH averaged at 46.3 points on a scale from 0 to 80. Children with higher socioeconomic status—as measured by both household income and educational level—started with higher (healthier) baseline scores. Students with high parental educational level had higher KAH scores (average of 47.2) than those with low parental educational level (average of 45.7). Children from high-income households had better KAH scores (47.4) than children from low-income households (45.8). Children from families with high educational level and household income had a lower zBMI compared with children from families with low educational level and household income at baseline.
After the end of the intervention, researchers compared KAH and zBMI between intervention and control groups. Overall, KAH improved more in the intervention group than in controls, and went up by 4.76 points compared to the control group after four months. There was also a bigger jump in points among children with higher socioeconomic status. KAH for the high-household-income intervention group went up by 6.33 more points than the control group. KAH for low-household-income intervention students went up 4.24 points more than the control group. KAH for intervention students from high-education families went up by 4.96 compared to the control group, and 3.75 for those from low-education families, suggesting that children from these families did not follow the curriculum as well as those from high-education backgrounds. zBMI numbers did not significantly change after the intervention and there were no major differences in zBMI between socioeconomic groups.
Dr. Fuster and his team are now running this school program in two boroughs of New York City and plan to expand it across the five boroughs in the next few years. This project will evaluate many other factors about health, teacher’s motivation, environment (pollution), and familial issues.
The FAMILIA project in the United States was funded by a grant from the American Heart Association and the Stephen Gellman Children’s Outreach Program The work in Spain and Colombia was funded by the SHE Foundation, the “la Caixa” Foundation. The project in Colombia was funded by the Santo Domingo Foundation.
Mount Sinai Heart is one of the nation’s top 4 hospitals in Cardiology/Heart Surgery
Mount Sinai Heart ranks No. 1 in New York and No. 4 globally according to Newsweek’s “The World’s Best Specialized Hospitals.” The Mount Sinai Hospital is also No. 1 in New York for cardiology, cardiac surgery, and vascular surgery, according to U.S. News & World Report®.
It is part of Mount Sinai Health System, which is New York City's largest academic medical system, encompassing eight hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. We advance medicine and health through unrivaled education and translational research and discovery to deliver care that is the safest, highest-quality, most accessible and equitable, and the best value of any health system in the nation. The Health System includes approximately 7,400 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report's® “Best Hospitals” Honor Roll for 2023-2024.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.

Valentin Fuster, MD, PhD, Receives Prestigious Award from City of Barcelona, Spain
Jan 23, 2023 View All Press Releases