After 30 years With a Heart Condition, a Long Island Father of Two Has a Life-Changing Heart Transplant
When in 1992, Bob Gorish, then 32, decided to donate blood, the blood bank noticed some irregularities in his heartbeat. An appointment with a cardiologist at a local hospital diagnosed cardiomyopathy—a degenerative disease of the heart muscle that can cause irregular heart rhythm and lead to heart failure. Bob, a father of two, had no obvious signs of heart problems before the diagnosis, but would go on to endure 30 years of health problems caused by his condition.
Ultimately, Bob’s journey led him to a life-changing heart transplant at Mount Sinai Fuster Heart Hospital—and a chance for a new life.
He initially underwent an electrophysiology study (a series of tests that check for abnormal heart rhythms) and was prescribed metoprolol, a “beta blocker” drug that treats chest pain and high blood pressure. But by 2006, his condition had deteriorated to a level where he needed to have a defibrillator implanted to protect from abnormal dangerous rhythms and regulate his heart beat. Over the next 18 years, he had four replacement defibrillators placed. He also underwent a series of ablations (a procedure that creates tiny scars in the heart to regulate heartbeat and prevent dangerous rhythms).
In 2006, Bob had a major stroke, which was likely a result of his heart muscle function being weak. The stroke initially left him with cognitive impairment, but speech therapy at a local hospital and a program of retraining at home, which he followed rigorously, helped him regain his cognitive abilities.
In 2010, genetic testing revealed that Bob was suffering from a rare form of cardiomyopathy called arrhythmogenic right ventricular cardiomyopathy (ARVC). ARVC is a genetic disease in which fatty fibrous tissue replaces normal heart muscle. This can cause irregular heart rhythms.
Seeing an expert in heart function
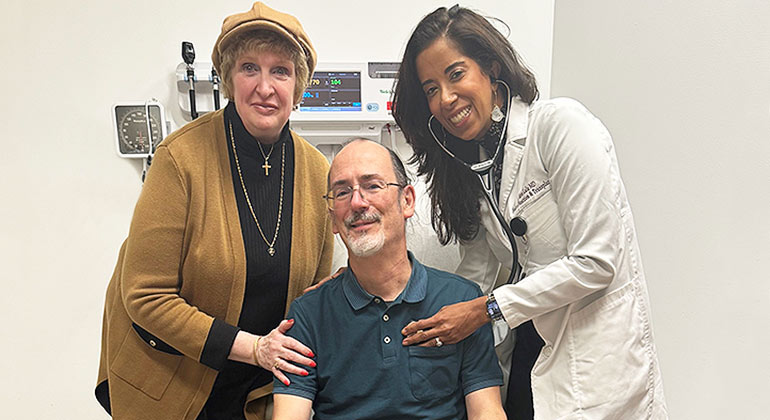
By 2019, Bob was showing signs of heart failure: he had gained more than 20 pounds from water retention, and was suffering from extreme fatigue and shortness of breath. In June 2019, he was referred to Anu Lala, MD, Associate Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai. Dr. Lala specializes in the diagnosis and treatment of a condition that she and other experts often prefer to call heart function, instead of heart failure—to emphasize hope and empowerment for patients. She prescribed Bob with a number of medications to help improve his heart function and symptoms.
”When I met Bob, his heart muscle function was indeed very weak and needed specialized care,” Dr. Lala says. “Understandably, both he and his wife were concerned about what this condition would mean in terms of quality and quantity of life years ahead.”
During that first visit, Bob and his wife, Diane, were impressed by Dr. Lala’s professionalism and openness. “From the moment we first met her, we liked her,” Bob says. “From that point forward, she was just on board and upfront. She engaged us with every aspect of decision-making.”
The medications stabilized Bob’s condition, and he was able to return to work, lose the water weight, and start walking regularly for at least a mile a day. However, as heart failure is a chronic condition that can progress over time, Dr. Lala also arranged for an assessment for heart transplant eligibility. In January 2020, he was assessed by Anelechi Anyanwu, MD, Vice Chair and Professor of Cardiovascular Surgery at Icahn Mount Sinai, and a renowned specialist in heart transplantation. Bob was put on the heart transplant list at status six—a lower level of priority due to his relative stability at the time.
Transplant priority rises
For the next few years, Bob’s condition remained stable, and he continued to build up his strength with walking and light exercise and by attending sessions at Mount Sinai South Nassau’s Cardiac Rehabilitation Program. However, in September 2023, while Bob was being prepared for a routine colonoscopy at Mount Sinai South Nassau, his heart went into a ventricular tachycardia, when the lower chamber of the heart beats too fast to pump well and the body is unable to receive enough oxygenated blood, triggering his defibrillator to give him a shock.
Days later, he was transferred to The Mount Sinai Hospital in a serious condition. The cardiology team performed a right heart catheterization (a procedure that provides information on blood flow and pressure levels in and around the heart) which showed progression of his heart failure. Dr. Lala and Dr. Anyanwu discussed Bob’s condition among the heart team, and the decision was made to raise his priority level for transplant and keep him in hospital until a new heart was available. In the meantime, Dr. Anyanwu and his team placed Bob on an extracorporeal membrane oxygenation (ECMO) device to support Bob’s heart and lungs.
The wait for a viable heart for transplant can take a number of months, but after fifteen days, the good news came that a heart was available for Bob. The transplant surgery took place on September 20 and took 10 hours.
Bob was discharged from hospital after three weeks and has been making steady progress ever since. He has been working again with Mount Sinai South Nassau’s heart rehabilitation program to build up his strength and stamina, and for the first time in 30 years, he is able to properly lift weights and exercise.
“Physically, I’m trying to put myself back on track. Even though I wasn’t on my back all that long waiting for the transplant, it still took a long time to recover, and I was weak in a lot of ways to start with. But I got back into the cardiac rehab program and that really helped—I am pretty strong now. I would definitely say as a recommendation for anyone who has a transplant, to get onto a cardiac rehab program to help them.”
“Active and free of fear”
Dr. Lala is also very happy with his progress. ”No words can express the joy we feel in seeing our patients regain function in their daily lives. For Bob to be able to be active and free of fear from being shocked by a defibrillator is just wonderful. In the process, I have made two friends.”
Diane and Bob are still in regular contact with the Mount Sinai transplant team, and emphasize how accessible and well organized the team has been throughout Bob’s transplant journey. “The nurses on the units, as well as the transplant team and the transplant coordinators have all been phenomenal,” Diane says. “They are always open to questions, and there's always somebody that will respond back to us, even if it's off hours.”
Bob’s is very grateful for being given this opportunity for a new life after transplant surgery and shares just how special it is to receive this type of surgery.
“I would like to share an anecdote—and it's probably common with people who have had transplants. After a couple of months, it was a Sunday and I remember waking up and I could feel and hear my heartbeat, which I couldn’t really do prior to the transplant, and it just felt good. But then I had this thought—that heart wasn’t yours. Believe me, it was emotional.”
“I said to him that's true, but it is your heart now,” Diane says. “We don’t know anything about the donor yet, but what he and his family decided to do is a beautiful thing. It gave me my husband back.”