Chronic lymphocytic leukemia (CLL)
CLL; Leukemia - chronic lymphocytic (CLL); Blood cancer - chronic lymphocytic leukemia; Bone marrow cancer - chronic lymphocytic leukemia; Lymphoma - chronic lymphocytic leukemia
Chronic lymphocytic leukemia (CLL) is cancer of a type of white blood cells called lymphocytes. These cells are found in the bone marrow and other parts of the body. Bone marrow is the soft tissue in the center of bones that helps form all blood cells.
CLL causes a slow increase in a certain type of white blood cells called B lymphocytes, or B cells. Cancer cells spread through the blood and bone marrow. CLL can also affect the lymph nodes or other organs such as the liver and spleen. CLL eventually can cause the bone marrow to lose its function.
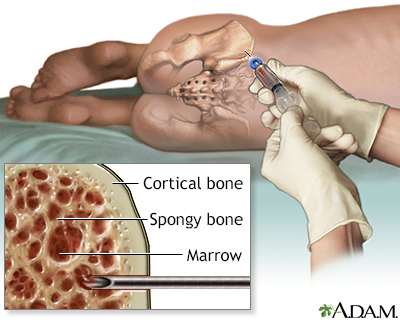
A small amount of bone marrow is removed during a bone marrow aspiration. The procedure is uncomfortable, but can be tolerated by both children and adults. The marrow can be studied to determine the cause of anemia, the presence of leukemia or other malignancy, or the presence of some storage diseases, in which abnormal metabolic products are stored in certain bone marrow cells.
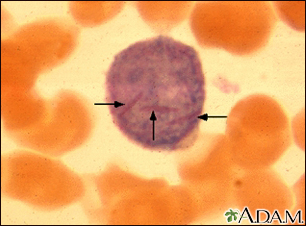
Note multiple Auer rods which are found only in acute myeloid leukemias, either myeloblastic or monoblastic. These rods consist of clumps of azurophilic granule material.
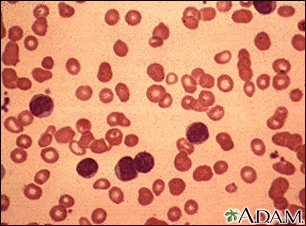
This is a microscopic view of bone marrow from a person with chronic lymphocytic leukemia. It shows predominantly small, mature lymphocytes.
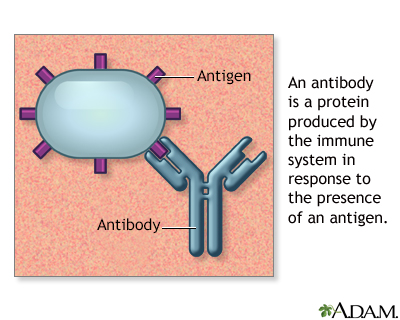
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Causes
The cause of CLL is unknown. There is no link to radiation exposure. It is unclear if certain chemicals can cause CLL. Exposure to Agent Orange during the Vietnam War has been linked to a slight increased risk for developing CLL.
CLL usually affects older adults, especially those over age 60. People under age 45 rarely develop CLL. CLL is more common in white people than in people of other races. It is more common in men than in women. Some people with CLL have family members with the disease.
Symptoms
Symptoms usually develop slowly. CLL often does not cause symptoms at first. It may be found by blood tests done in people for other reasons.
Symptoms of CLL may include:
- Enlarged lymph nodes, liver, or spleen
- Excessive sweating, night sweats
- Fatigue
- Fever
- Infections that keep coming back (recur), despite treatment
- Loss of appetite or becoming full too quickly (early satiety)
- Weight loss
Exams and Tests
Your health care provider will perform a physical exam and ask about your symptoms.
Tests to diagnose CLL may include:
- Complete blood count (CBC) with blood cell differential.
- Flow cytometry test of the white blood cells.
- Fluorescent in situ hybridization (FISH) is used to look at and count genes or chromosomes. This test may help diagnose CLL or guide treatment.
- Testing for other gene changes may help predict how well the cancer will respond to treatment.
People with CLL usually have a high white blood cell count.
Tests that look at changes in the DNA inside the cancer cells may also be done. Results from these tests and from staging tests help your provider determine your treatment.
Treatment
If you have early stage CLL, your provider will just monitor you closely. Treatment is not generally given for early-stage CLL, unless you have:
- Infections that keep coming back
- Leukemia that is rapidly getting worse
- Low red blood cell or platelet counts
- Fatigue, loss of appetite, weight loss, or night sweats
- Swollen lymph nodes
Targeted therapy and sometimes chemotherapy are used to treat CLL. Your provider will determine which type of medicines are right for you.
Blood transfusions or platelet transfusions may be required if blood counts are low.
Bone marrow or stem cell transplantation may be used in younger people with advanced or high-risk CLL. A transplant is the only therapy that offers a potential cure for CLL, but it also has risks. Your provider will discuss the risks and benefits with you.
You and your provider may need to manage other concerns during your leukemia treatment, including:
- Managing your pets during chemotherapy
- Bleeding problems
- Dry mouth
- Eating enough calories
- Safe eating during cancer treatment
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
Your provider can discuss with you the outlook of your CLL based on its stage and how well it responds to treatment.
Possible Complications
Complications of CLL and its treatment may include:
- Autoimmune hemolytic anemia, a condition in which red blood cells are destroyed by the immune system.
- Bleeding from low platelet count.
- Hypogammaglobulinemia, a condition in which there is a lower level of antibodies than normal, which can increase the risk of infection.
- Idiopathic thrombocytopenic purpura (ITP), a bleeding disorder.
- Infections that keep coming back (recur).
- Fatigue that can range from mild to severe.
- Other cancers, including a much more aggressive lymphoma (Richter transformation).
- Side effects of targeted therapy and chemotherapy.
When to Contact a Medical Professional
Contact your provider if you develop enlarged lymph nodes or unexplained fatigue, bruising, excessive sweating, or weight loss.
References
Awan FT, Byrd JC. Chronic lymphocytic leukemia. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff''s Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 99.
National Cancer Institute website. Chronic lymphocytic leukemia treatment (PDQ) - health professional version.
National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology. Chronic lymphocytic leukemia/small lymphocytic lymphoma. Version 3. 2024.
Version Info
Last reviewed on: 3/31/2024
Reviewed by: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
