Bone marrow transplant
Transplant - bone marrow; Stem cell transplant; Hematopoietic stem cell transplant; Reduced intensity nonmyeloablative transplant; Mini transplant; Allogenic (or allogeneic) bone marrow transplant; Autologous bone marrow transplant; Umbilical cord blood transplant; Aplastic anemia - bone marrow transplant; Leukemia - bone marrow transplant; Lymphoma - bone marrow transplant; Multiple myeloma - bone marrow transplant
A bone marrow transplant is a procedure to replace damaged or diseased bone marrow with healthy bone marrow stem cells.
Bone marrow is the soft, fatty tissue inside your breastbone (sternum) and pelvic bones. Your bone marrow produces blood cells. Stem cells in your bone marrow give rise to all of your different blood cells.
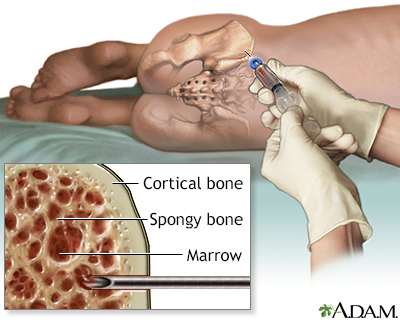
A small amount of bone marrow is removed during a bone marrow aspiration. The procedure is uncomfortable, but can be tolerated by both children and adults. The marrow can be studied to determine the cause of anemia, the presence of leukemia or other malignancy, or the presence of some storage diseases, in which abnormal metabolic products are stored in certain bone marrow cells.
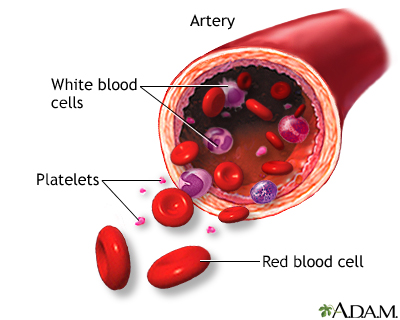
Blood transports oxygen and nutrients to body tissues and returns waste and carbon dioxide. Blood distributes nearly everything that is carried from one area in the body to another place within the body. For example, blood transports hormones from endocrine organs to their target organs and tissues. Blood helps maintain body temperature and normal pH levels in body tissues. The protective functions of blood include clot formation and the prevention of infection.
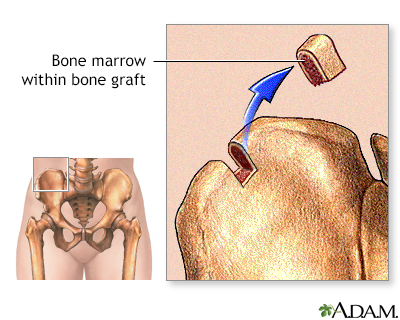
Bone marrow may be harvested from the hip (iliac bone) to serve as bone grafts elsewhere in the body.
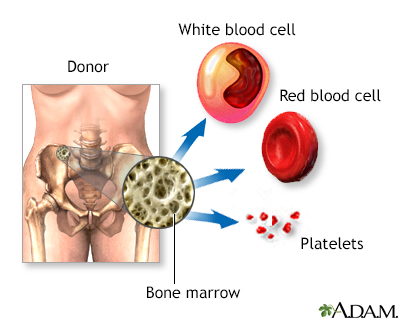
Bone-marrow is a soft, fatty tissue found inside of bones that produces blood cells (red blood cells, white blood cells, and platelets). Red blood cells carry oxygen throughout the body. White blood cells act to ward off infection. Platelets aid in blood-clotting.
Description
Before the transplant, chemotherapy, radiation, or both may be given. This may be done in two ways:
- Ablative (myeloablative) treatment -- High-dose chemotherapy, radiation, or both are given to kill any cancer cells. This also kills all healthy bone marrow that remains, and allows new stem cells to grow in the bone marrow.
- Reduced intensity treatment, also called a mini transplant -- Lower doses of chemotherapy and radiation are given before a transplant. This allows older people, and those with other health problems to have a transplant.
There are four kinds of bone marrow transplants:
- Autologous bone marrow transplant -- The term auto means self. Stem cells are removed from you before you receive high-dose chemotherapy or radiation treatment. The stem cells are stored in a freezer. After high-dose chemotherapy or radiation treatments, your stem cells are put back in your body to make normal blood cells. This is called a rescue transplant.
- Allogeneic bone marrow transplant -- The term allo means other. Stem cells are removed from another person, called a donor. Most times, the donor's genes must at least partly match your genes. Special tests are done to see if a donor is a good match for you. A brother or sister is most likely to be a good match. Sometimes parents, children, and other relatives are good matches. Donors who are not related to you, yet still match, may be found through national bone marrow registries.
- Umbilical cord blood transplant -- This is a type of allogeneic transplant. Stem cells are removed from a newborn baby's umbilical cord right after birth. The stem cells are frozen and stored until they are needed for a transplant. Umbilical cord blood cells are very immature so there is less of a need for perfect matching. Due to the smaller number of stem cells, blood counts take much longer to recover.
- Haploidentical transplant -- This is a type of allogeneic transplant, in which the donor is not completely matched with the recipient. A haploidentical transplant may be from a family member. Children are always a half-match for their parents, and parents are a half-match for their children. Siblings have a 50% chance of being a half-match for each other. Special treatments are performed to decrease the chance of complications due to the incomplete match.
A stem cell transplant is usually done after chemotherapy and radiation is complete. The stem cells are delivered into your bloodstream, usually through a tube called a central venous catheter. The process is similar to getting a blood transfusion. The stem cells travel through the blood into the bone marrow.
Donor stem cells can be collected in two ways:
- Bone marrow harvest -- This minor surgery is done under general anesthesia. This means the donor will be asleep and pain-free during the procedure. The bone marrow is removed from the back of both hip bones. The amount of marrow removed depends on the weight of the person who is receiving it. This method is rarely performed today.
- Leukapheresis -- First, the donor is given several days of shots to help stem cells move from the bone marrow into the blood. During leukapheresis, blood is removed from the donor through an IV line. The part of white blood cells that contains stem cells is then separated in a machine and removed to be later given to the recipient. The red blood cells are returned to the donor.
Why the Procedure Is Performed
A bone marrow transplant replaces bone marrow that is either not working properly or has been destroyed (ablated) by chemotherapy or radiation. For many cancers, the donor's white blood cells may attack any remaining cancer cells, which are seen as foreign, similar to when white cells attack bacteria or viruses when fighting an infection.
Your health care provider may recommend a bone marrow transplant if you have:
- Certain cancers, such as leukemia, lymphoma, myelodysplasia, or multiple myeloma.
- A disease that affects the production of bone marrow cells, such as aplastic anemia, congenital neutropenia, severe immune system illnesses, sickle cell anemia, or thalassemia.
Risks
A bone marrow transplant may cause the following symptoms:
- Chest pain
- Drop in blood pressure
- Fever, chills, flushing
- Headache
- Hives
- Nausea
- Pain
- Shortness of breath
- Strange taste in the mouth
Possible complications of a bone marrow transplant depend on many things, including:
- Your age
- Your overall health
- How good of a match your donor was
- The type of bone marrow transplant you received (autologous, allogeneic, or umbilical cord blood)
Complications may include:
- Anemia
- Bleeding in the lungs, intestines, brain, and other areas of the body
- Cataracts
- Clotting in the small veins of the liver
- Damage to the kidneys, liver, lungs, and heart
- Delayed growth in children who receive a bone marrow transplant
- Early menopause
- Graft failure, which means that the new cells do not settle into the body and start producing stem cells
- Graft-versus-host disease (GVHD), a condition in which the donor cells attack your own body
- Infections, which can be very serious
- Inflammation and soreness in the mouth, throat, esophagus, and stomach, called mucositis
- Pain
- Stomach or abdominal problems, including diarrhea, nausea, and vomiting
Before the Procedure
Your provider will ask about your medical history and do a physical exam. You will have many tests before treatment begins.
Before transplant, you will have 1 or 2 tubes, called central venous catheters, inserted into a blood vessel in your neck or arms. This tube allows you to receive treatments, fluids, and sometimes nutrition. It is also used to draw blood.
Your provider will likely discuss the emotional stress of having a bone marrow transplant. You may want to meet with a counselor. It is important to talk to your family and children to help them understand what to expect.
You will need to make plans to help you prepare for the procedure and handle tasks after your transplant:
- Complete an advance care directive
- Arrange medical leave from work
- Take care of bank or financial statements
- Arrange care of pets
- Arrange for someone to help with household chores
- Confirm health insurance coverage
- Pay bills
- Arrange for care of your children
- Find housing for yourself or your family near the hospital, if needed
After the Procedure
A bone marrow transplant is usually done in a hospital or medical center that specializes in such treatment. Most of the time, you stay in a special bone marrow transplant unit in the center. This is to limit your chance of getting an infection.
Depending on the treatment and where it is done, all or part of an autologous or allogeneic transplant may be done as an outpatient. This means you do not have to stay in the hospital overnight.
How long you stay in the hospital depends on:
- Whether you developed any complications related to the transplant
- The type of transplant
- Your medical center's procedures
While you are in the hospital:
- Your health care team will closely monitor your blood count and vital signs.
- You will receive medicines to prevent GVHD and prevent or treat infections, including antibiotics, antifungals, and antiviral medicine.
- You will likely need many blood transfusions.
- You will be fed through a vein (IV) until you can eat by mouth, and stomach side effects and mouth sores have gone away.
After you leave the hospital, be sure to follow instructions on how to care for yourself at home.
Outlook (Prognosis)
How well you do after the transplant depends on:
- The type of bone marrow transplant
- How well the donor's cells match yours
- What type of cancer or illness you have
- Your age and overall health
- The type and dosage of chemotherapy or radiation therapy you had before your transplant
- Any complications you may have
A bone marrow transplant may completely or partially cure your illness. If the transplant is a success, you can go back to most of your normal activities as soon as you feel well enough. Usually it takes up to 1 year to recover fully, depending on what complications occur.
Complications or failure of the bone marrow transplant can lead to death.
References
American Cancer Society website. How stem cell and bone marrow transplants are used to treat cancer.
Im A, Pavletic SZ. Hematopoietic stem cell transplantation. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 28.
Zubair AC, Rowley SD. Practical aspects of hematopoietic stem cell harvesting and mobilization. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 102.
Version Info
Last reviewed on: 2/2/2023
Reviewed by: Mark Levin, MD, Hematologist and Oncologist, Monsey, NY. Review provided by VeriMed Healthcare Network. Internal review and update on 07/17/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
