Common peroneal nerve dysfunction
Common fibular nerve dysfunction; Neuropathy - common peroneal nerve; Peroneal nerve injury; Peroneal nerve palsy; Fibular neuropathy
Common peroneal nerve dysfunction is due to damage to the peroneal nerve leading to loss of movement or sensation in the foot and leg. This condition is also called common fibular nerve dysfunction.
Blood clot formation in the veins is called venous thrombosis. Venous thrombosis most commonly forms in the veins of the legs. Risk factors for venous thrombosis include prolonged bed rest or immobility, as can be necessary after surgery, cancer, and estrogen therapy.
Causes
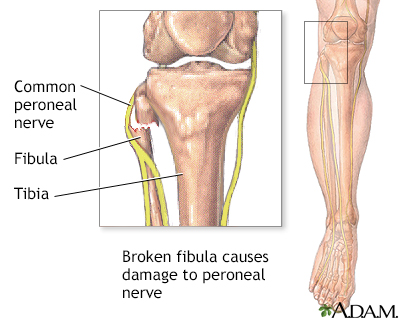
The common peroneal nerve is a branch of the sciatic nerve. It supplies movement and sensation to the lower leg, foot and toes. Common peroneal nerve dysfunction is a type of peripheral neuropathy (nerve damage outside the brain or spinal cord). This condition can affect people of any age.
Common peroneal nerve is a type of mononeuropathy. Mononeuropathy is nerve damage to a single nerve. Certain body-wide conditions can also cause single nerve injuries.
Damage to the nerve disrupts the myelin sheath that covers the axon (branch of the nerve cell). The axon can also be injured, which is a more severe injury that causes similar symptoms.
Common causes of damage to the common peroneal nerve include the following:
- Trauma or injury to the knee
- Fracture of the fibula (a bone of the lower leg)
- Use of a tight plaster cast (or other long-term constriction) of the lower leg
- Crossing the legs regularly
- Regularly wearing high boots
- Pressure to the knee from positions during deep sleep or coma
- Injury during knee surgery or from being placed in an awkward position during anesthesia
Common peroneal nerve injury is often seen in people:
- Who are very thin (for example, from anorexia nervosa)
- Who have certain autoimmune conditions, such as polyarteritis nodosa
- Who have nerve damage from other medical problems, such as diabetes, excess alcohol use, or inherited nerve disorders
Symptoms
When the nerve is injured and results in dysfunction, symptoms may include:
- Decreased sensation, numbness, or tingling in the top of the foot or the outer part of the upper or lower leg
- Foot that drops (unable to hold the foot up)
- "Slapping" gait (walking pattern in which each step makes a slapping noise)
- Toes drag while walking
- Walking problems
- Weakness of the ankles or feet
- Loss of muscle mass because the nerves aren't stimulating the muscles
Exams and Tests
Your health care provider will perform a physical exam, which may show:
- Loss of muscle control in the lower legs and feet
- Atrophy (thinning or loss) of the foot or foreleg muscles
- Difficulty lifting up the foot and toes and making toe-out movements
Tests of nerve activity include:
- Electromyography (EMG), a test of electrical activity in muscles)
- Nerve conduction tests (to see how fast electrical signals move through a nerve)
- Magnetic resonance imaging (MRI)
- Nerve ultrasound
Other tests may be done depending on the suspected cause of nerve dysfunction, and the person's symptoms and how they develop. Tests may include blood tests, x-rays and scans.
Treatment
Treatment aims to improve mobility and independence. Any illness or other cause of the neuropathy should be treated. Padding the knee may prevent further injury by crossing the legs, while also serving as a reminder to not cross your legs.
In some cases, corticosteroids injected into the area may reduce swelling and pressure on the nerve.
Surgery may help reduce symptoms in some cases. It may be needed:
- To relieve pressure on the nerve if the disorder is caused by pressure on the nerve
- To remove tumors pressing on the nerve
You may need surgery if:
- The disorder does not go away
- You have problems with movement
- There is evidence that the nerve axon is damaged
CONTROLLING SYMPTOMS
You may need over-the-counter or prescription pain relievers to control pain. Other medicines that may be used to reduce pain include:
- Gabapentin
- Carbamazepine
- Tricyclic antidepressants, such as amitriptyline
If your pain is severe, a pain specialist can help you explore all options for pain relief.
Physical therapy exercises may help you maintain muscle strength.
Orthopedic devices may improve your ability to walk and prevent contractures. These may include:
- Braces
- Splints
- Orthopedic shoes or other equipment
Vocational counseling, occupational therapy, or similar programs may help you stay as mobile and independent as possible.
Outlook (Prognosis)
The outcome depends on the cause of the problem. Successfully treating the cause may relieve the dysfunction, but it may take several months for the nerve to improve.
Severe nerve damage may cause permanent disability. The nerve pain may be very uncomfortable. This disorder does not usually shorten a person's expected lifespan.
Possible Complications
Problems that may develop with this condition include:
- Decreased ability to walk
- Permanent decrease in sensation in the legs or feet
- Permanent weakness or paralysis in the legs or feet
- Side effects of medicines
When to Contact a Medical Professional
Contact your provider if you have symptoms of common peroneal nerve dysfunction.
Prevention
Avoid crossing your legs or putting long-term pressure on the back or side of the knee. Treat injuries to the leg or knee right away.
If a cast, splint, dressing, or other pressure on the lower leg causes a tight feeling or numbness, call your provider.
References
Katirji B. Disorders of peripheral nerves. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 106.
Toro DRD, Seslija D, King JC. Fibular (peroneal) neuropathy. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 75.
Version Info
Last reviewed on: 8/28/2023
Reviewed by: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
