Drug-induced pulmonary disease
Interstitial lung disease - drug induced
Drug-induced pulmonary disease is lung disease brought on by a bad reaction to a medicine. Pulmonary means related to the lungs.
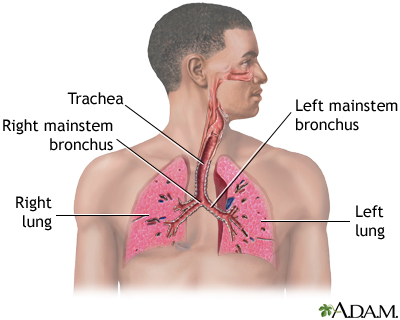
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Causes
Many types of lung injury can result from medicines. It is usually impossible to predict who will develop lung disease from a medicine.
Types of lung problems or diseases that may be caused by medicines include:
- Allergic reactions -- asthma, hypersensitivity pneumonitis, or eosinophilic pneumonia
- Bleeding into the lung air sacs, called alveoli (alveolar hemorrhage)
- Swelling and inflamed tissue in the main passages that carry air to the lungs (bronchitis)
- Damage to lung tissue (interstitial fibrosis)
- Drugs that cause the immune system to mistakenly attack and destroy healthy body tissue, such as drug-induced lupus erythematosus
- Granulomatous lung disease -- a type of inflammation in the lungs
- Inflammation of the lung air sacs (pneumonitis or infiltration)
- Lung vasculitis (inflammation of lung blood vessels)
- Lymph node swelling
- Swelling and irritation (inflammation) of the chest area between the lungs (mediastinitis)
- Abnormal buildup of fluid in the lungs (pulmonary edema)
- Buildup of fluid between the layers of tissue that line the lungs and chest cavity (pleural effusion)
- Abnormal pressure of the arteries that bring blood to the lungs (pulmonary hypertension)
Many medicines and substances are known to cause lung disease in some people. These include:
- Antibiotics, such as nitrofurantoin and sulfa drugs
- Heart medicines, such as amiodarone
- Chemotherapy drugs such as bleomycin, cyclophosphamide, and methotrexate
- Immunotherapy drugs that are used to treat cancer
- Street drugs
Symptoms
Symptoms may include any of the following:
Exams and Tests
The health care provider will perform a physical exam and listen to your chest and lungs with a stethoscope. Abnormal breath sounds may be heard.
Tests that may be done include:
- Arterial blood gases
- Blood test to check for an autoimmune disorder
- Blood chemistry
- Bronchoscopy
- Complete blood count with blood differential
- Chest CT scan
- Chest x-ray
- Lung biopsy (in rare cases)
- Lung function tests
- Thoracentesis (if pleural effusion is present)
Treatment
The first step is to stop the medicine that is causing the problem. Other treatments depend on your specific symptoms. For example, you may need oxygen until the drug-induced lung disease improves. Anti-inflammatory medicines called corticosteroids are most often used to quickly reverse the lung inflammation.
Outlook (Prognosis)
Acute episodes usually go away within 48 to 72 hours after the medicine has been stopped. Chronic symptoms may take longer to improve.
Some drug-induced lung diseases, such as pulmonary fibrosis, may never go away and can worsen, even after the medicine or substance is stopped and can lead to severe lung disease and death.
Possible Complications
Complications that may develop include:
- Diffuse interstitial pulmonary fibrosis
- Hypoxemia (low blood oxygen)
- Respiratory failure
When to Contact a Medical Professional
Contact your provider if you develop symptoms of this disorder.
Prevention
Note any past reaction you have had to a medicine, so that you can avoid the medicine in the future. Wear a medical alert bracelet if you have known drug reactions. Stay away from street drugs.
References
Kurian ST, Walker CM, Chung JH. Drug-induced lung disease. In: Walker CM, Chung JH, eds. Muller's Imaging of the Chest. 2nd ed. Philadelphia, PA: Elsevier; 2019:chap 65.
Limper AH. Drug-induced pulmonary disease. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 99.
Version Info
Last reviewed on: 5/3/2023
Reviewed by: Denis Hadjiliadis, MD, MHS, Paul F. Harron, Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
