Kaposi sarcoma
Kaposi's sarcoma; HIV - Kaposi; AIDS - Kaposi; Kaposi's sarcoma
Kaposi sarcoma (KS) is a cancerous tumor of the cells that make up blood vessels and lymph nodes.
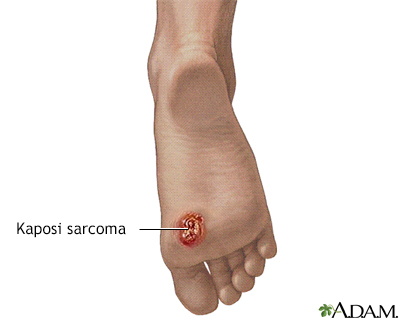
Kaposi sarcoma lesion on the foot. This once-rare malignancy of the blood vessels is now associated with AIDS. It is more frequently associated with AIDS in homosexual men than AIDS in IV drug users. The malignancy results in purplish grape-like lesions in the skin, gastrointestinal tract and other organs.
Kaposi sarcoma was once a rare malignancy of the blood vessels but is now associated with AIDS. It is more frequently associated with AIDS in homosexual men than AIDS in IV drug users. Recent research has suggested that this malignancy may be caused by a newly discovered herpes virus. The malignancy results in purplish, grape-like lesions in the skin, gastrointestinal tract, and other organs.

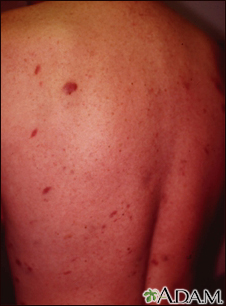
Kaposi sarcoma was once a rare malignancy of the blood vessels but is now associated with AIDS. It is more frequently associated with AIDS in homosexual men than AIDS in IV drug users. The malignancy results most frequently in purplish to reddish-purple flat or grape-like lesions in the skin, gastrointestinal tract, and other organs.

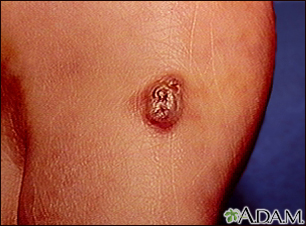
Kaposi sarcoma, seen here on the thigh, was once a rare malignancy of the blood vessels, but is now associated with AIDS. It is more frequently associated with AIDS in homosexual men than AIDS in IV drug users. The malignancy results in purplish to reddish-purple grape-like lesions in the skin, gastrointestinal tract, and other organs.

Kaposi sarcoma usually occurs in male homosexuals with AIDS. These lesions can appear anywhere on the body as purple, elevated growths. This sarcoma is located near the anus (perianal).
Kaposi sarcoma is a malignant tumor of the connective tissue.
Causes
KS is the result of an infection with a gamma herpesvirus known as Kaposi sarcoma-associated herpesvirus (KSHV), or human herpesvirus 8 (HHV8). It is in the same family as the Epstein-Barr virus, which causes mononucleosis.
KSHV is transmitted mainly through saliva. It can also be spread through sexual contact, blood transfusion, or transplants. After it enters the body, the virus can infect different kinds of cells, especially cells that line blood vessels and lymphatic vessels. Like all herpesviruses, KSHV remains in your body for the rest of your life. If your immune system becomes weakened in the future, this virus may have the chance to reactivate, causing symptoms.
There are four types of KS based on the groups of people who are infected:
- Classic KS: Mainly affects older men of Eastern European, Middle Eastern, and Mediterranean descent. The disease usually develops slowly.
- Epidemic (AIDS-related) KS: Occurs most often in people who have HIV infection and have developed AIDS.
- Endemic (African) KS: Mainly affects people of all ages in Africa.
- Immunosuppression-associated, or transplantation-associated, KS: Occurs in people who have had an organ transplant and take medicines that suppress their immune system.
Symptoms
The tumors (lesions) most often appear as bluish-red or purple bumps on the skin. They are reddish-purple because they are rich in blood vessels.
The lesions may first appear on any part of the body. They also can appear inside the body. Lesions inside the body may bleed. Lesions in the lungs can cause bloody sputum or shortness of breath.
Exams and Tests
Your health care provider will perform a physical exam, focusing on the lesions.
The following tests may be performed to diagnose KS and associated conditions:
Treatment
How KS is treated depends on:
- How much the immune system is suppressed (immunosuppression)
- Number and location of the tumors
- Symptoms
Treatments include:
- Antiviral therapy against HIV, since there is no specific therapy for HHV-8
- Combination chemotherapy
- Freezing the lesions
- Radiation therapy
Lesions may return after treatment.
Outlook (Prognosis)
Treating KS does not improve the chances of survival from HIV/AIDS itself. The outlook depends on the person's immune status and how much of the HIV virus is in their blood (viral load). If HIV is controlled with medicine, the lesions will often shrink away on their own.
Possible Complications
Complications can include:
- Cough (possibly bloody) and shortness of breath if the disease is in the lungs
- Leg swelling that may be painful or cause infections if the disease is in the lymph nodes of the legs
The tumors can return even after treatment. KS can be deadly for a person with AIDS.
An aggressive form of endemic KS can spread quickly to the bones. Another form found in African children does not affect the skin. Instead, it spreads through the lymph nodes and vital organs, and can quickly become deadly.
Prevention
Safer sexual practices can prevent HIV infection. This prevents HIV/AIDS and its complications, including KS.
KS almost never occurs in people with HIV/AIDS whose disease is well controlled.
References
Kaye KM. Kaposi sarcoma-associated herpesvirus (human herpesvirus 8). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 140.
Merrick ST, Glesby MJ. Systemic manifestations of HIV/AIDS. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 359.
National Cancer Institute website. Kaposi sarcoma treatment (PDQ) - health professional version.
Version Info
Last reviewed on: 11/10/2024
Reviewed by: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
