Placental insufficiency
Placental dysfunction; Uteroplacental vascular insufficiency; Oligohydramnios
The placenta is the link between you and your baby. When the placenta does not work as well as it should, your baby can get less oxygen and nutrients from you. As a result, your baby may:
- Not grow well
- Show signs of fetal stress (this means the baby's heart does not work normally)
- Have a harder time during labor
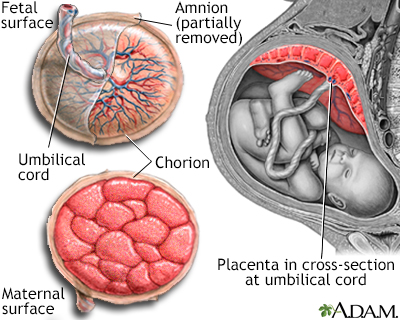
The placenta provides the fetus with oxygen and nutrients and takes away waste such as carbon dioxide via the umbilical cord.
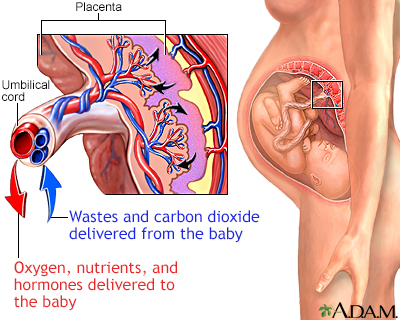
In the placenta, nutrients, wastes, and gases are exchanged between the mothers blood and the babys blood.
Causes
The placenta may not work well, either due to pregnancy problems or social habits. These may include:
- Diabetes
- Going past your due date
- High blood pressure during pregnancy (called preeclampsia)
- Medical conditions that increase the mother's chances of blood clots
- Smoking
- Taking cocaine or other illicit drugs
- Anemia
Certain medicines can also increase the risk for placental insufficiency.
In some cases, the placenta:
- May have an abnormal shape
- May not grow big enough (more likely if you are carrying twins or other multiples)
- Does not attach correctly to the surface of the womb
- Breaks away from the surface of the womb or bleeds prematurely
Symptoms
A woman with placental insufficiency usually does not have any symptoms. However, certain diseases, such as preeclampsia, which can be symptomatic, can cause placental insufficiency.
Exams and Tests
Your health care provider will measure the size of your growing womb (uterus) at each visit, starting about halfway through your pregnancy.
If your uterus is not growing as expected, a pregnancy ultrasound will be done. This test will measure your baby's size and growth, and assess the size and placement of the placenta.
Other times, problems with the placenta or your baby's growth may be found on a routine ultrasound that is done during your pregnancy.
Either way, your provider will order tests to check how your baby is doing. The tests may show that your baby is active and healthy, and the amount of amniotic fluid is normal. Or, these tests can show that the baby is having problems.
You may be asked to keep a daily record of how often your baby moves or kicks.
Treatment
The next steps your provider will take depend on:
- The results of tests
- Your due date
- Other problems that may be present, such as high blood pressure or diabetes
If your pregnancy is less than 37 weeks and the tests show that your baby is not under too much stress, your provider may decide to wait longer. Sometimes you may need to get more rest. You will have tests often to make sure your baby is doing well. Treating high blood pressure or diabetes may also help improve your baby's growth.
If your pregnancy is over 37 weeks or tests show your baby is not doing well, your provider may want to deliver your baby. Labor may be induced (you will be given medicine to make labor start), or you may need a cesarean delivery (C-section).
Outlook (Prognosis)
Problems with the placenta can affect the developing baby's growth. The baby cannot grow and develop normally in the womb if it does not get enough oxygen and nutrients.
Possible Complications
Complications associated with placental insufficiency may include:
- Preeclampsia
- Preterm labor
- Intrauterine growth restriction (IUGR)
- Placental abruption or premature separation of the placenta
- Decreased oxygen delivery to the baby at birth
- Increased risk for fetal loss
Prevention
Getting prenatal care early in pregnancy will help make sure that the mother is as healthy as possible during the pregnancy.
Smoking, alcohol, and other recreational drugs can interfere with the baby's growth. Avoiding these substances may help prevent placental insufficiency and other pregnancy complications.
References
Benson AE, Branch DW. Collagen vascular diseases in pregnancy. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 51.
Mari G, Resnik R. Fetal growth restriction. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 44.
Rampersad R, Macones GA. Late- and postterm pregnancy. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 29.
Version Info
Last reviewed on: 10/15/2024
Reviewed by: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
