Sclerosing cholangitis
Primary sclerosing cholangitis; PSC
Sclerosing cholangitis refers to swelling (inflammation), scarring, and destruction of the
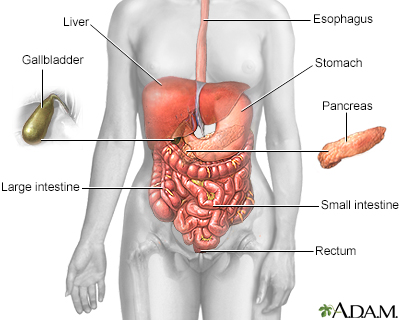
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
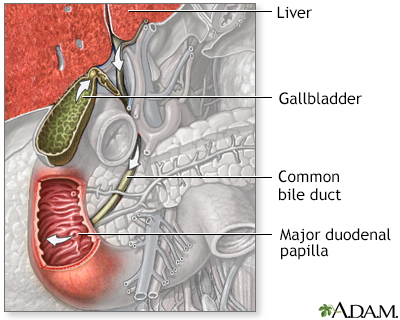
The biliary system is comprised of the organs and duct system that create, transport, store and release bile into the duodenum for digestion. Includes the liver, gallbladder and bile ducts (named the cystic, hepatic, common, and pancreatic duct).
Causes
The cause of this condition is unknown in most cases.
The disease may be seen in people who have:
- Inflammatory bowel disease (IBD) such as ulcerative colitis and Crohn disease
- Autoimmune disorders
- Chronic pancreatitis (inflamed pancreas)
- Sarcoidosis (a disease that causes inflammation in various parts of the body)
Genetic factors may also be responsible. Sclerosing cholangitis occurs more often in men than women. This disorder is rare in children.
Sclerosing cholangitis may also be caused by:
- Choledocholithiasis (gallstones in the bile duct)
- Infections in the liver, gallbladder, and bile ducts
Symptoms
The first symptoms are usually:
- Fatigue
- Itching
- Yellowing of the skin and eyes (jaundice)
However, some people have no symptoms.
Other symptoms may include:
- Enlarged liver
- Enlarged spleen
- Loss of appetite and weight loss
- Repeat episodes of cholangitis (an infection of the bile duct that causes fever, jaundice and pain in the right upper abdomen)
Exams and Tests
Even though some people do not have symptoms, blood tests shows that they have abnormal liver function. Your health care provider will look for:
- Diseases that cause similar problems
- Diseases that often occur with this condition (especially IBD)
- Gallstones
Tests that show cholangitis include:
- Abdominal CT scan
- Abdominal ultrasound
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Liver biopsy
- Magnetic resonance cholangiopancreatography (MRCP)
- Percutaneous transhepatic cholangiogram (PTC)
- Blood tests for liver enzymes (liver function tests)
Treatment
Medicines that may be used include:
- Cholestyramine (such as Prevalite) to treat itching
- Ursodeoxycholic acid (ursodiol) to improve liver function
- Fat-soluble vitamins (D, E, A, K) to replace what is lost from the disease itself
- Antibiotics to treat infections in the bile ducts
These surgical procedures may be done:
- Inserting a long, thin tube with a balloon at the end to open up narrowing (endoscopic balloon dilation of strictures)
- Placement of a drain or tube for major narrowing (strictures) of bile ducts
- Proctocolectomy (removal of colon and rectum, for those who have both ulcerative colitis and sclerosing cholangitis) does not affect the progression of primary sclerosing cholangitis (PSC)
- Liver transplant
Outlook (Prognosis)
How well people do varies. The disease tends to get worse over time. Sometimes people develop:
- Ascites (buildup of fluid in the space between the lining of the abdomen and abdominal organs) and varices in the esophagus or stomach (enlarged veins)
- Biliary cirrhosis (liver scarring due to inflammation of the bile ducts)
- Liver failure
- Persistent jaundice
Some people develop infections of the bile ducts that keep returning.
People with this condition have a high risk for developing cancer of the bile ducts (cholangiocarcinoma). They should be checked regularly with a liver imaging test and blood tests. People who also have IBD may have an increased risk for developing cancer of the colon or rectum and should have periodic colonoscopy.
Possible Complications
Complications may include:
- Bleeding esophageal varices
- Cancer in the bile ducts (cholangiocarcinoma)
- Cirrhosis and liver failure
- Infection of the biliary system (cholangitis)
- Narrowing of the bile ducts
- Vitamin deficiencies
References
Ahrendt GM, Ahrendt SA. Gallbladder and biliary tree: Management of primary sclerosing cholangitis. In: Cameron AM, Cameron JL, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:457-538.
Bowlus C, Assis DN, Goldberg D. Primary and secondary sclerosing cholangitis. In: Sanyal AJ, Boyer TD, Lindor KD, Terrault NA, eds. Zakim and Boyer's Hepatology. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 43.
Levy C, Bowlus CL. Primary and secondary sclerosing cholangitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 68.
Version Info
Last reviewed on: 5/2/2023
Reviewed by: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
