Chronic pancreatitis
Chronic pancreatitis - chronic; Pancreatitis - chronic - discharge; Pancreatic insufficiency - chronic; Acute pancreatitis - chronic
Pancreatitis is swelling of the pancreas. Chronic pancreatitis is present when this problem does not heal or recurs and does not improve, gets worse over time, and leads to permanent damage.
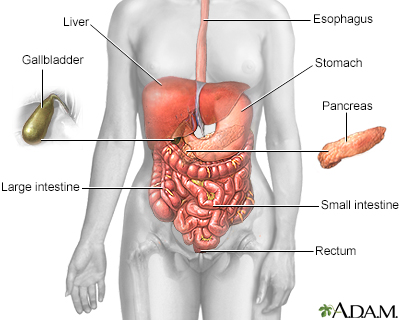
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
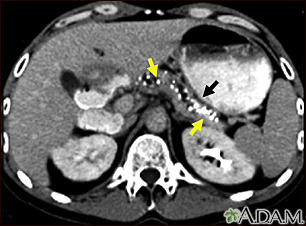
CT scan of the upper abdomen showing multiple white-colored calcifications. These occur in chronic pancreatitis.
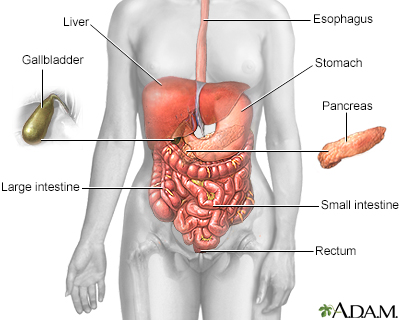
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
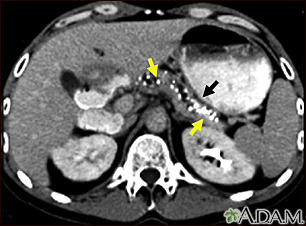
CT scan of the upper abdomen showing multiple white-colored calcifications. These occur in chronic pancreatitis.
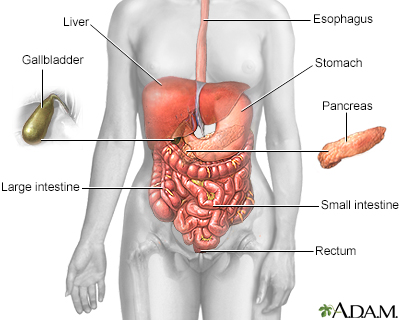
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
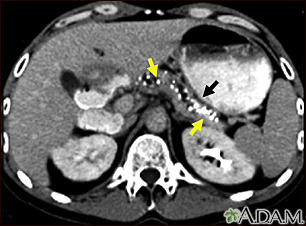
CT scan of the upper abdomen showing multiple white-colored calcifications. These occur in chronic pancreatitis.
Causes
The pancreas is an organ located behind the stomach. It produces chemicals (called enzymes) needed to digest food. It also produces the hormones insulin and glucagon.
When scarring of the pancreas occurs, the organ is no longer able to make the right amount of these enzymes. As a result, your body may be unable to digest fat and key elements of food.
Damage to the parts of the pancreas that make insulin may lead to diabetes mellitus.
The condition is most often caused by alcohol abuse over many years. Repeated episodes of acute pancreatitis can lead to chronic pancreatitis. Genetics may be a factor in some cases. Sometimes, the cause is not known or caused by gall stones.
Other conditions that have been linked to chronic pancreatitis:
- Problems when the immune system attacks the body
- Blockage of the tubes (ducts) that drain enzymes from the pancreas
- Cystic fibrosis
- High levels of a fat, called triglycerides, in the blood
- Overactive parathyroid gland
- Use of certain medicines (especially sulfonamides, thiazides, and azathioprine)
- Pancreatitis that is passed down in families (hereditary)
Chronic pancreatitis is more common in men than in women. This often occurs in people ages 30 to 40.
Symptoms
Symptoms include:
- Greatest in the upper abdomen
- May last from hours to days; over time, may always be present
- May get worse from eating
- May get worse from drinking alcohol
- May also be felt in the back as if it is boring through the abdomen
DIGESTIVE PROBLEMS
- Chronic weight loss, even when eating habits and amounts are normal.
- Diarrhea, nausea, and vomiting.
- Foul-smelling fatty or oily stools.
- Pale or orange-colored stools.
- Chronic pancreatitis can lead to pancreatic cancer.
Exams and Tests
Tests to diagnose pancreatitis include:
- Fecal fat test
- Increased serum amylase level
- Increased serum lipase level
- Serum trypsinogen
Tests that may show the cause of pancreatitis include:
- Serum IgG4 (for diagnosing autoimmune pancreatitis)
- Gene testing, most often done when other common causes are not present or there is a family history
Imaging tests that can show swelling, scarring, calcifications or other changes of the pancreas may be seen on:
- CT scan of the abdomen
- Ultrasound of the abdomen
- Endoscopic ultrasound (EUS)
- Magnetic resonance cholangiopancreatography (MRCP)
- Endoscopic retrograde cholangiopancreatography (ERCP)
ERCP is a procedure that looks at your bile and pancreatic ducts. It is done through an endoscope.
Treatment
People with severe pain or who are losing weight may need to stay in the hospital for:
- Pain medicines.
- Fluids given through a vein (IV).
- Stopping food or fluid by mouth to limit the activity of the pancreas, and then slowly starting an oral diet. Feeding the intestine is an important part of treating pancreatitis. If you can’t eat by mouth, a temporary feeding tube may be placed to give your intestine nutrients.
- Inserting a tube through the nose or mouth to remove the contents of the stomach (nasogastric suctioning) may sometimes be done. The tube may stay in for 1 to 2 days, or sometimes for 1 to 2 weeks.
The right diet is important for people with chronic pancreatitis to keep a healthy weight and get the correct nutrients. A nutritionist can help you create a diet that includes:
- Drinking plenty of liquids
- Limiting fats
- Eating small, frequent meals (this helps reduce digestive symptoms)
- Getting enough vitamins and calcium in the diet, or as extra supplements
- Limiting caffeine
The health care provider may prescribe pancreatic enzymes. You must take these medicines with every meal, and even with snacks. The enzymes will help you digest food better, gain weight and reduce diarrhea.
Avoiding smoking and drinking alcoholic beverages is very important, even if your pancreatitis is mild. This helps decrease your risk of pancreatitis and pancreatic cancer.
Other treatments may involve:
- Pain medicines or a surgical nerve block to relieve pain
- Taking insulin to control blood sugar (glucose) level
Surgery may be performed if a blockage is found. In severe cases, a part of or the entire pancreas may be removed.
Outlook (Prognosis)
This is a serious disease that may lead to disability and death. You can reduce the risk by avoiding alcohol.
Possible Complications
Complications may include:
- Ascites (build up of fluid in the abdomen)
- Blockage (obstruction) of the small intestine or bile ducts
- Blood clot in the vein of the spleen
- Fluid collections in the pancreas (pancreatic pseudocysts) that may become infected (pancreatic abscess)
- Diabetes
- Poor absorption of fat, nutrients, and vitamins (most often the fat-soluble vitamins, A, D, E, or K)
- Iron deficiency anemia
- Vitamin B12 deficiency
When to Contact a Medical Professional
Contact your provider if:
- You develop symptoms of pancreatitis
- You have pancreatitis, and your symptoms get worse or do not improve with treatment
Prevention
Finding the cause of acute pancreatitis and treating it quickly may help prevent chronic pancreatitis. Limit the amount of alcohol you drink to reduce your risk of developing this condition.
References
Forsmark CE. Chronic pancreatitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 59.
Forsmark CE. Pancreatitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 130.
Price MD, Walsh CM, Makary MA. Management of chronic pancreatitis. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:541-545.
Van Buren G, Fisher WE. Acute and chronic pancreatitis. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:175-182.
Version Info
Last reviewed on: 12/31/2023
Reviewed by: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
