Thrombophlebitis
Phlebitis; Deep vein thrombosis - thrombophlebitis; Thrombophilia - thrombophlebitis
Thrombophlebitis is swelling (inflammation) of a vein. A blood clot (thrombus) in the vein is the most common cause of this swelling.

This picture shows a red and swollen thigh and leg caused by a blood clot (thrombus) in the deep veins in the groin (iliofemoral veins) which prevents normal return of blood from the leg to the heart.
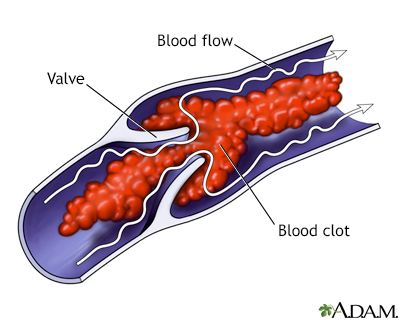
Deep venous thrombosis (DVT) affects mainly the veins in the lower leg and the thigh. It involves the formation of a clot (thrombus) in the larger veins of the area.
Causes
Thrombophlebitis may affect deeper, larger veins or veins near the skin surface. Most of the time, it occurs in the pelvis and legs.
Blood clots may form when something slows or changes the flow of blood in the veins. Risk factors include:
- A pacemaker catheter that has been passed through the vein in the groin
- Bed rest or sitting in one position for too long, such as plane travel
- Family history of blood clots, which may imply the presence of inherited disorders that lead to increased risk of clots. Common ones include deficiency or lack of antithrombin 3, protein C, and protein S, factor V Leiden (FVL) and prothrombin abnormalities
- Fractures in the pelvis or legs
- Giving birth within the last 6 months
- Pregnancy
- Obesity
- Recent surgery (most commonly hip, knee, or female pelvic surgery)
- Too many blood cells being made by the bone marrow, causing the blood to be thicker than normal (polycythemia vera)
- Having an indwelling (long-term) catheter in a blood vessel
Blood is more likely to clot in someone who has certain problems or disorders, such as:
- Cancer
- Certain autoimmune disorders, such as lupus
- Cigarette smoking
- Conditions that make it more likely to develop blood clots
- Taking estrogens or birth control pills (this risk is even higher with smoking)
Symptoms
Thrombophlebitis often causes the following symptoms:
- Swelling in the part of the body affected
- Pain in the part of the body affected
- Skin redness (not always present)
- Warmth and tenderness over the vein
Exams and Tests
The health care provider can often diagnose the condition based on how the affected area looks. Your provider will frequently check your vital signs. This is to make sure you don't have complications.
If the cause cannot be easily identified, one or more of the following tests may be done:
- Blood coagulation studies
- Doppler ultrasound
- Venography
- Genetic testing
Treatment
Support stockings and wraps can help to reduce discomfort. Your provider may prescribe medicines such as:
- Painkillers
- Blood thinners to prevent new clots from forming, most often only prescribed when deep veins are involved
- Medicines such as ibuprofen to reduce pain and swelling
- Medicines injected into the vein to dissolve an existing clot
You may be told to do the following:
- Keep pressure off the area to reduce pain and decrease the risk for further damage.
- Raise the affected area to reduce swelling.
Rare treatment options are:
- Surgical removal of a vein near the surface
- Vein stripping
- Bypass of the vein
Outlook (Prognosis)
Prompt treatment can treat thrombophlebitis and its other forms.
Possible Complications
Complications of thrombophlebitis include:
- Blood clot in the lungs (pulmonary embolism)
- Chronic pain at the location of the thrombophlebitis
- Chronic swelling at the location of the thrombophlebitis
When to Contact a Medical Professional
Contact your provider if you have symptoms of thrombophlebitis.
Contact your provider right away if:
- Your symptoms do not improve with treatment.
- Your symptoms get worse.
- New symptoms occur (such as an entire limb becoming pale, cold, or swollen).
Prevention
Routine changing of intravenous (IV) lines helps to prevent thrombophlebitis related to IVs.
If you are taking a long car or plane trip:
- Walk or stretch your legs once in a while
- Drink plenty of liquids
- Wear support hose
If you are hospitalized, your provider may prescribe medicine to prevent thrombophlebitis.
References
Wasan S. Superficial thrombophlebitis and its management. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 151.
Weitz JI, Eikelboom JW. Venous thrombosis and embolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 68.
Version Info
Last reviewed on: 2/8/2024
Reviewed by: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
