Trichomoniasis
Trichomonas vaginitis; STD - trichomonas vaginitis; STI - trichomonas vaginitis; Sexually transmitted infection - trichomonas vaginitis; Cervicitis - trichomonas vaginitis
Trichomoniasis is a sexually transmitted infection caused by the parasite Trichomonas vaginalis.
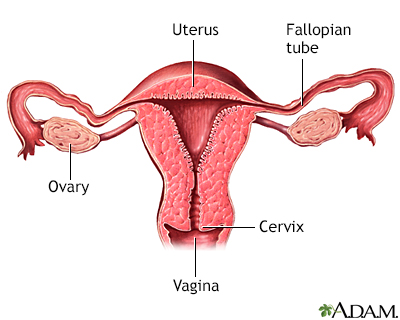
The uterus is a muscular organ with thick walls, two upper openings to the fallopian tubes and an inferior opening to the vagina.
Causes
Trichomoniasis ("trich") is found worldwide. In the United States, most cases occur in women between ages 16 and 35 years. Trichomonas vaginalis is spread through sexual contact with an infected partner, either through penis-to-vagina intercourse or vulva-to-vulva contact. The parasite cannot survive in the mouth or rectum.
The disease can affect both men and women, but the symptoms differ. The infection usually does not cause symptoms in men and goes away on its own in a few weeks.
Symptoms
Women may have these symptoms:
- Discomfort with intercourse
- Itching of the inner thighs
- Vaginal discharge (thin, greenish-yellow, frothy or foamy)
- Vaginal or vulvar itching, or swelling of the labia
- Vaginal odor (foul or strong smell)
Men who have symptoms may have:
- Burning after urination or ejaculation
- Itching of the urethra
- Slight discharge from the urethra
Occasionally, some men with trichomoniasis may develop:
- Swelling and irritation in the prostate gland (prostatitis).
- Swelling in the epididymis (epididymitis), the tube that connects the testicle with the vas deferens. The vas deferens connects the testicles to the urethra.
Exams and Tests
In women, a pelvic examination shows red blotches on the vaginal wall or cervix. Examining the vaginal discharge under a microscope may show signs of inflammation or infection-causing germs in vaginal fluids. A Pap test may also diagnose the condition, but is not required for diagnosis.
The disease can be hard to diagnose in men. Men are treated if the infection is diagnosed in any of their sexual partners. They may also be treated if they keep having symptoms of urethral burning or itching, even after getting treatment for gonorrhea and chlamydia.
Treatment
Antibiotics, most often metronidazole (Flagyl) or tinidazole (Tindamax), are commonly used to cure the infection.
Do not drink alcohol while taking the medicine and for 48 hours afterward. Doing so can cause:
- Severe nausea
- Abdominal pain
- Vomiting
Avoid sexual intercourse until you have finished treatment. Your sexual partners should be treated at the same time, even if they have no symptoms. If you have been diagnosed with a sexually transmitted infection (STI), you should be screened for other STIs.
Outlook (Prognosis)
With proper treatment, you are likely to fully recover.
Possible Complications
Long-term infection may cause changes in the tissue on the cervix. These changes may be seen on a routine Pap smear. Treatment should be started and the Pap test should be repeated 3 to 6 months later.
Treating trichomoniasis helps prevent it from spreading to sexual partners. Trichomoniasis is more common among people with HIV/AIDS.
This condition has been linked to premature delivery in pregnant women. More research about trichomoniasis in pregnancy is still needed.
When to Contact a Medical Professional
Contact your health care provider if you have any unusual vaginal discharge or irritation.
Also, call if you suspect that you have been exposed to the disease.
Prevention
Practicing safer sex can help reduce the risk of sexually transmitted infections, including trichomoniasis.
Other than total abstinence, condoms remain the best and most reliable protection against sexually transmitted infections. Condoms must be used consistently and correctly to be effective.
References
Abdallah M, Augenbraun MH, McCormack W. Vulvovaginitis and cervicitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 108.
Centers for Disease Control and Prevention website. Trichomoniasis. About trichomoniasis.
Telford SR, Krause PJ. Babesiosis and other protozoan diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 324.
Version Info
Last reviewed on: 11/10/2024
Reviewed by: Jatin M. Vyas, MD, PhD, Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
