Diabetes and exercise
Exercise - diabetes; Exercise - type 1 diabetes; Exercise - type 2 diabetes

A person with type 2 diabetes can use exercise to help control their blood sugar levels and provide energy their muscles need to function throughout the day. By maintaining a healthy diet and sufficient exercise, a person with type 2 diabetes may be able to keep their blood sugar in the normal non-diabetic range without medicine.
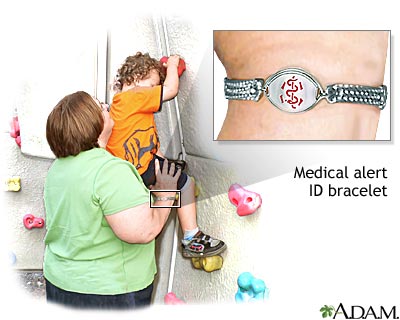
People with diabetes, seizure disorders, or heart disease should always wear a medical alert bracelet or necklace that emergency medical workers will be able to find. Medical identification products can help ensure proper treatment in an emergency.

People with diabetes are prone to foot problems because the disease can cause damage to the blood vessels and nerves, which may result in decreased ability to sense a trauma to the foot. The immune system is also altered, so that the person with diabetes cannot efficiently fight infection.
Exercise will Help Your Diabetes
Exercise can help lower your blood sugar without medicines. It reduces your risk of heart disease. Exercise can also lessen the symptoms of depression and reduce stress.
But be patient. It may take several months of regular exercising before you see changes in your health. It is important to understand that exercise can benefit your health even if it does not cause much weight loss.
Talk to Your Doctor First
Your health care provider should make sure your exercise program is safe for you. An exercise program is safe for most people with diabetes. Your provider may ask about symptoms, such as shortness of breath, chest pain, or leg pain that you may get when you walk upstairs or up a hill. In rare cases, your provider will order tests to make sure that you can exercise safely without damaging your heart.
If you take medicines that lower your blood sugar, exercise can make your blood sugar go too low. Talk to your provider or nurse about how to take your medicines when you exercise or how to adjust the doses to prevent low blood sugars.
Some types of vigorous exercise can make your eyes worse if you already have diabetic eye disease. Get an eye exam before starting a new exercise program.
After you start your exercise program, contact your provider if you have any of the following:
- Feel faint, have chest pain, or feel short of breath when you exercise
- Feel pain or numbness in your feet. Also contact your provider if you have sores or blisters on your feet
- Your blood sugar gets too low or too high during or after exercising
Getting Started
Start with walking. If you are out of shape, start by walking for 5 to 10 minutes a day.
Try to set a goal of fast walking. You should do this for 30 to 45 minutes, at least 5 days a week. In order to lose weight, the amount of exercise may need to be greater. So do more if you can. Swimming or exercise classes are also good.
If you don't have a safe place to walk, or have pain when walking, you can start with body weight exercises in your home. Talk to your provider about which exercises are right for you.
Wear a bracelet or necklace that says you have diabetes. Tell coaches and exercise partners that you have diabetes. Always have fast-acting sources of sugar with you, such as juice or hard candy. Carry a cell phone with emergency phone numbers with you, as well.
Drink plenty of water. Do this before, during, and after exercising. Try to exercise at the same time of day, for the same amount of time, and at the same level. This will make your blood sugar easier to control. If your schedule is less regular, exercising at different times of the day is still better than not exercising at all.
Try to avoid sitting for more than 30 minutes at a time. Get up and stretch. Walk or do some quick exercises like lunges, squats, or wall push-ups.
Your Blood Sugar and Exercise
The blood sugar response to exercise is not always easy to predict. Different types of exercises can make blood sugar go up or down. Most of the time, your response to any specific exercise will be the same. Testing your blood sugar more often is the safest plan.
Check your blood sugar before you exercise. Also, check it during exercise if you are working out for more than 45 minutes, especially if this is an exercise you have not done regularly.
Check your blood sugar again right after exercise, and later on. Exercise can cause your blood sugar to decrease for up to 12 hours after you are done.
If you use insulin, ask your provider when and what you should eat before you exercise. Also, find out how to adjust your insulin dose when you exercise.
Do not inject insulin in a part of your body that you are exercising, such as the shoulders or thighs.
Keep a snack nearby that can raise your blood sugar quickly. Examples are:
- Five or six small soft candies
- One tablespoon (tbsp), or 15 grams, of sugar, plain or dissolved in water
- One tbsp, or 15 milliliters (mL) of honey or syrup
- Three or four glucose tablets
- One half of a 12-ounce can (355 mL) of regular, non-diet soda or sports drink
- One half cup (4 ounces or 118 mL) of fruit juice
Have a larger snack if you will be exercising more than usual. You can also have more frequent snacks. You may need to adjust your medicine if you are planning unusual exercise.
If exercise frequently causes your blood sugar to be low, talk with your provider. You may need to lower the dose of your medicine.
Your Feet and Exercise
Always check your feet and shoes for any problems before and after exercise. You might not feel pain in your feet because of your diabetes. You may not notice a sore or blister on your foot. Contact your provider if you notice any changes on your feet. Small problems can become serious if they go untreated.
Wear socks that keep moisture away from your feet. Also, wear comfortable, well-fitting shoes.
If you have redness, swelling and warmth across the middle of your foot or ankle after exercise let your provider know right away. This can be a sign of a joint problem that is more common in people with diabetes, called Charcot foot.
References
American Diabetes Association Professional Practice Committee. 5. Facilitating positive health behaviors and well-being to improve health outcomes: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S77-S110. Erratum in: Diabetes Care. 2024;47(4):761-762. PMID: 38078584
Dhatariya KK, Umpierrez GE, Crandall JP. Diabetes. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 210.
Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S76-S99. PMID: 24222015
Lundgren JA, Kirk SE. The athlete with diabetes. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 18.
Version Info
Last reviewed on: 5/20/2024
Reviewed by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
