Managing your blood sugar
Hyperglycemia - control; Hypoglycemia - control; Diabetes - blood sugar control; Blood glucose - managing
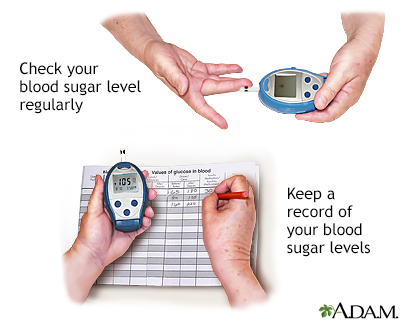
Checking your blood sugar levels often and recording the results will tell you how well you are managing your diabetes so you can stay as healthy as possible. The best times to check your blood sugar are before meals and at bedtime. Your blood sugar meter may have software to help you track your blood sugar level. This is usually available from the manufacturer's website. This is usually available from the manufacturer's website. There are websites available to store your blood sugar data so your health care provider can access it more easily. Ask your provider if this might help your diabetes be better controlled.
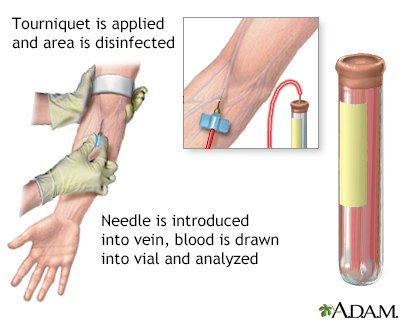
Blood is drawn from a vein (venipuncture), usually from the inside of the elbow or the back of the hand. A needle is inserted into the vein, and the blood is collected in an air-tight vial or a syringe. Preparation may vary depending on the specific test.
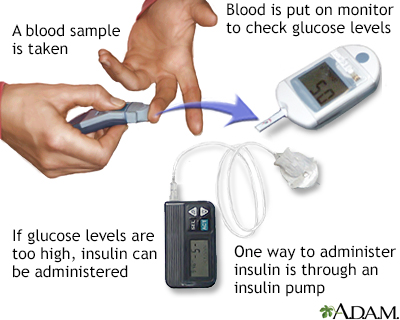
A person with diabetes constantly manages their blood's sugar (glucose) levels. After a blood sample is taken and tested, it is determined whether the glucose levels are low or high. If glucose levels are too low carbohydrates are ingested. If glucose in the blood is too high, the appropriate amount of insulin is administered into the body such as through an insulin pump.
Take Control of Your Diabetes
Know the basic steps for managing your diabetes. Poorly managed diabetes can lead to many health problems.
Know how to:
- Recognize and treat low blood sugar (hypoglycemia)
- Recognize and treat high blood sugar (hyperglycemia)
- Plan healthy meals
- Monitor your blood sugar (glucose)
- Take care of yourself when you are sick
- Find, buy, and store diabetes supplies
- Get the checkups you need
If you take insulin, you should also know how to:
- Give yourself insulin
- Adjust your insulin doses and the foods you eat to manage your blood sugar during exercise and on sick days
You should also live a healthy lifestyle.
- Exercise at least 30 minutes a day, 5 days a week. In addition, do muscle strengthening exercises 2 or more days a week.
- Avoid sitting for more than 30 minutes at a time.
- Try speed walking, swimming, or dancing. Pick an activity you enjoy. Always check with your health care provider before starting any new exercise programs.
- Follow your meal plan. Every meal is an opportunity to make a good choice for your diabetes management.
Take your medicines the way your provider recommends.
Diabetes is on the rise worldwide, and is a serious, lifelong disease that can lead to heart disease, stroke, and lasting nerve, eye and foot problems. Let's talk about diabetes and the difference between the three types of diabetes. So, what exactly is diabetes and where does it come from? An organ in your body called the pancreas produces insulin, a hormone that controls the levels of your blood sugar. When you have too little insulin in your body, or when insulin doesn't work right in your body, you can have diabetes, the condition where you have abnormally high glucose or sugar levels in your blood. Normally when you eat food, glucose enters your bloodstream. Glucose is your body's source of fuel. Your pancreas makes insulin to move glucose from your bloodstream into muscle, fat, and liver cells, where your body turns it into energy. People with diabetes have too much blood sugar because their body cannot move glucose into fat, liver, and muscle cells to be changed into and stored for energy. There are three major types of diabetes. Type 1 diabetes happens when the body makes little or no insulin. It usually is diagnosed in children, teens, or young adults. But about 80% of people with diabetes have what's called Type 2 diabetes. This disease often occurs in middle adulthood, but young adults, teens, and now even children are now being diagnosed with it linked to high obesity rates. In Type 2 diabetes, your fat, liver, and muscle cells do not respond to insulin appropriately. Another type of diabetes is called gestational diabetes. It's when high blood sugar develops during pregnancy in a woman who had not had diabetes beforehand. Gestational diabetes usually goes away after the baby is born. But, still pay attention. These women are at a higher risk of type 2 diabetes over the next 5 years without a change in lifestyle. If you doctor suspects you have diabetes, you will probably have a hemoglobin A1c test. This is an average of your blood sugar levels over 3 months. You have pre-diabetes if your A1c is 5.7% to 6.4%. Anything at 6.5% or higher indicates you have diabetes. Type 2 diabetes is a wake up call to focus on diet and exercise to try to control your blood sugar and prevent problems. If you do not control your blood sugar, you could develop eye problems, have problems with sores and infections in your feet, have high blood pressure and cholesterol problems, and have kidney, heart, and problems with other essential organs. People with Type 1 diabetes need to take insulin every day, usually injected under the skin using a needle. Some people may be able to use a pump that delivers insulin to their body all the time. People with Type 2 diabetes may be able to manage their blood sugar through diet and exercise. But if not, they will need to take one or more drugs to lower their blood sugar levels. The good news is, people with any type of diabetes, who maintain good control over their blood sugar, cholesterol, and blood pressure, have a lower risk of kidney disease, eye disease, nervous system problems, heart attack, and stroke, and can live, a long and healthy life.
Check Your Blood Sugar Often
Checking your blood sugar levels often and writing down, or using an app to track the results will tell you how well you are managing your diabetes. Talk to your provider and diabetes educator about how often you should check your blood sugar.
- Not everyone with diabetes needs to check their blood sugar every day. But some people may need to check it many times a day.
- If you have type 1 diabetes, check your blood sugar at least 4 times a day.
Usually, you will test your blood sugar before meals and at bedtime. You may also check your blood sugar:
- If you are having symptoms of low blood sugar (hypoglycemia)
- After you eat out, particularly if you have eaten foods you don't normally eat
- If you feel sick
- Before or after you exercise
- If you have been under a lot of stress
- If you eat too much or skip meals or snacks
- If you are taking new medicines, took too much insulin or diabetes medicine by mistake, or took your medicine at the wrong time
- If your blood sugar has been higher or lower than normal
- If you are drinking alcohol
Keep a record for yourself and your provider. This will be a big help if you are having problems managing your diabetes. It will also tell you what works and what doesn't work, to keep your blood sugar under control. Write down:
- The time of day
- Your blood sugar level
- The amount of carbohydrates you ate
- The type and dose of your diabetes medicines
- The type of exercise you do and for how long
- Anything unusual, such as feeling stressed, eating different foods, or being sick
Many glucose meters let you store this information.
You and your provider should set a target goal for your blood sugar levels for different times during the day. If your blood sugar is higher than your goals for 3 days and you don't know why, call your provider.
Random blood sugar values are often not that useful to your provider and this can be frustrating to people with diabetes. Often fewer values with more information (meal description and time, exercise description and time, medicine dose and time) related to the blood sugar value are much more useful to help guide medicine decisions and dose adjustments.
Recommended Blood Sugar Targets
For people with type 1 diabetes, the American Diabetes Association recommends that blood sugar targets be based on a person's needs and goals, including whether they are pregnant. Talk to your provider and diabetes educator about the best goals for you. General guidelines are:
Before meals, your blood sugar should be:
- From 90 to 130 mg/dL (5.0 to 7.2 mmol/L) for adults
- From 90 to 130 mg/dL (5.0 to 7.2 mmol/L) for children, 13 to 19 years old
- From 90 to 180 mg/dL (5.0 to 10.0 mmol/L) for children, 6 to 12 years old
- From 100 to 180 mg/dL (5.5 to 10.0 mmol/L) for children under 6 years old
After meals (1 to 2 hours after eating), your blood sugar should be:
- Less than 180 mg/dL (10 mmol/L) for adults
At bedtime, your blood sugar should be:
- From 90 to 150 mg/dL (5.0 to 8.3 mmol/L) for adults
- From 90 to 150 mg/dL (5.0 to 8.3 mmol/L) for children, 13 to 19 years old
- From 100 to 180 mg/dL (5.5 to 10.0 mmol/L) for children, 6 to 12 years old
- From 110 to 200 mg/dL (6.1 to 11.1 mmol/L) for children under 6 years old
For people with type 2 diabetes, the American Diabetes Association also recommends that blood sugar targets be individualized. Talk to your provider and diabetes educator about the best goals for you. General guidelines are:
Before meals, your blood sugar should be:
- From 80 to 130 mg/dL (4.4 to 7.2 mmol/L) for adults
After meals (1 to 2 hours after eating), your blood sugar should be:
- Less than 180 mg/dL (10.0 mmol/L) for adults
What to do When Your Blood Sugar is High or Low
High blood sugar can harm you. If your blood sugar is high, you need to know how to bring it down. Here are some questions to ask yourself if your blood sugar is high.
- Are you eating too much or too little? Have you been following your diabetes meal plan?
- Are you taking your diabetes medicines correctly?
- Has your provider (or insurance company) changed your medicines?
- Is your insulin expired? Check the date on your insulin.
- Has your insulin been exposed to very high or very low temperatures?
- If you take insulin, have you been taking the correct dose? Are you changing your syringes or pen needles?
- Are you afraid of having low blood sugar? Is that causing you to eat too much or take too little insulin or other diabetes medicine?
- Have you injected insulin into a firm, numb, bumpy, or overused area? Have you been rotating sites?
- Have you been less or more active than usual?
- Do you have a cold, flu, or another illness?
- Have you had more stress than usual?
- Have you been checking your blood sugar every day?
- Have you gained or lost weight?
When to Call the Doctor
Contact your provider if your blood sugar is too high or too low and you do not understand why. When your blood sugar is in your target range, you will feel better and your health will be better.
References
Atkinson MA, Mcgill DE, Dassau E, Laffel L. Type 1 diabetes. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 36.
American Diabetes Association Professional Practice Committee. 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S111-S125. PMID: 38078586
American Diabetes Association Professional Practice Committee. 14. Children and Adolescents: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S258-281. PMID: 38078582
Riddle MC, Ahmann AJ. Therapeutics of type 2 diabetes. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 35.
Version Info
Last reviewed on: 2/28/2024
Reviewed by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
