Hemorrhoid surgery
Hemorrhoidectomy
Hemorrhoids are swollen veins around the anus. They may be inside the anus (internal hemorrhoids) or outside the anus (external hemorrhoids).
Often hemorrhoids do not cause problems. But if hemorrhoids bleed a lot, cause pain, or become swollen, hard, and painful, surgery can remove them.
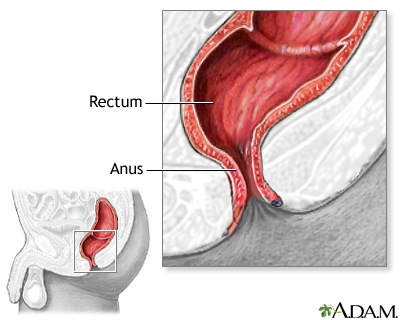
The rectum is the final portion of the large intestine. It empties stool from the body through the anus.
Description
Hemorrhoid surgery can be done in your surgeon's office or in the hospital operating room. In most cases, you can go home the same day. The type of surgery you have depends on your symptoms and the location and size of the hemorrhoid.
Before the surgery, your surgeon will numb the area so you can stay awake, but not feel anything. For some types of surgery, you may be given general anesthesia. This means you will be given medicine in your vein that puts you to sleep and keeps you pain-free during surgery.
Hemorrhoid surgery may involve:
- Putting a small rubber band around a hemorrhoid to shrink it by blocking blood flow.
- Stapling a hemorrhoid to block blood flow, causing it to shrink.
- Using a knife (scalpel) to remove hemorrhoids. You may or may not have stitches.
- Injecting a chemical into the blood vessel of the hemorrhoid to shrink it.
- Using a laser to burn the hemorrhoid.
Why the Procedure Is Performed
Often you can manage small hemorrhoids by:
- Eating a high fiber diet
- Drinking more water
- Avoiding constipation (taking a fiber supplement if needed)
- Not straining when you have a bowel movement
When these measures do not work and you are having bleeding and pain, your health care provider may recommend hemorrhoid surgery.
Risks
Risks for anesthesia and surgery in general are:
- Reactions to medicines, breathing problems
- Bleeding, blood clots, infection
Risks for this type of surgery include:
- Leaking a small amount of stool (long-term problems are rare)
- Problems passing urine because of the pain
Before the Procedure
Be sure to tell your surgeon:
- If you are or could be pregnant
- What medicines you are taking, including medicines, supplements, or herbs you bought without a prescription
- If you have been drinking a lot of alcohol, more than 1 or 2 drinks a day
During the days before the surgery:
- You may be asked to temporarily stop taking blood thinners such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), clopidogrel (Plavix), warfarin (Coumadin).
- Ask your surgeon which medicines you should still take on the day of your surgery.
- If you smoke, try to stop. Smoking can slow healing. Ask your provider for help quitting.
- Let your surgeon know about any cold, flu, fever, herpes breakout, or other illness you may have before your surgery. If you do get sick, your surgery may need to be postponed.
On the day of your surgery:
- Follow your surgeon's instructions about when to stop eating and drinking.
- Take any medicines you are asked to take with a small sip of water.
- Follow instructions on when to arrive at your surgeon's office or at the hospital. Be sure to arrive on time.
After the Procedure
You will usually go home the day of your surgery. Be sure you arrange to have someone drive you home. You may have a lot of pain after surgery as the area tightens and relaxes. You may be given medicines to relieve pain.
Follow instructions on how to care for yourself at home.
Outlook (Prognosis)
Most people do very well after hemorrhoid surgery. You should recover fully in a few weeks, depending on how involved the surgery was.
You will need to continue with diet and lifestyle changes to help prevent the hemorrhoids from coming back.
References
Abcarian AM, Abcarian H. Management of hemorrhoids. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:287-293.
Hyman N, Umanskiy K. Anus. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 53.
Version Info
Last reviewed on: 9/9/2023
Reviewed by: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
