Mount Sinai Researchers Track HIV in Real Time as it Infects and Spreads in Living Tissue
{To watch video of HIV-infected T cells in red interacting with uninfected T cells in green, click here. Notice the pausing of these green cells when in contact with the infected cell.}
By watching brightly glowing HIV-infected immune cells move within mice, researchers at the Icahn School of Medicine at Mount Sinai have shown how infected immune cells latch onto an uninfected sister cell to directly transmit newly minted viral particles. These interactions allow HIV to spread efficiently between these immune cells, known as CD4+ helper T cells. The research, published online today in Cell Reports, challenges the long-held perception that the primary route of HIV infection of immune cells is from free-floating viral particles that move within tissue and blood fluids.
While HIV cell-to-cell transmission has been observed in test tube experiments, this is the first study to capture these interactions in a living animal. Although cell-to-cell infection does result in release of abundant solo viral particles, direct transmission from HIV-infected immune cells to other cells — which can then replicate in clusters of these cells — is a much more efficient route to quickly spread the virus, researchers say. It may be particularly important in allowing the virus to spread in the body even before it is detectable in the blood.
Previous studies in cell culture have indicated that cell-to-cell infection may help HIV to resist antibodies and potent therapies. This study provides direct evidence that these interactions do occur in infected immune tissues, and highlight the importance of considering cell-to-cell transmission in developing new treatments.
“All HIV treatment to date has been based on the free-floating virion model,” says Benjamin K. Chen, MD, PhD, an Associate Professor of Infectious Diseases, Microbiology, and Immunology at the Icahn School of Medicine at Mount Sinai. “We believe that the sensitivity to antibodies used as potential HIV treatment and to certain antiretroviral drugs can be decreased by cell-to-cell transmission. Agents that efficiently block cell-to-cell transmission may help reduce the HIV viral reservoir, and vaccines that can neutralize this transmission may also help prevent or control HIV.”
HIV, or human immunodeficiency virus, is a virus that attacks the body’s immune system. If left untreated, HIV can progress and develop into AIDS (acquired immunodeficiency syndrome). More than 1.2 million people in the United States are living with HIV infection. Globally, more than 39 million people have been infected.
Glowing proteins track HIV movement
Lead author Kenneth M. Law, a graduate fellow in Dr. Chen’s laboratory, attached green fluorescent molecules derived from jellyfish and red glowing proteins from coral onto variants of HIV. The researchers then introduced the two strains into mice transplanted with a human immune system and watched in real time as HIV spread from one CD4+ helper T cell to another.
“We could visualize hot spots of infection within lymphoid tissue, which has millions of cells moving dynamically within the tissue,” says Mr. Law. “By focusing just on the green and red glowing cells, we could monitor how an infected cell influences uninfected cells.”
Using an advanced imaging technique called intravital microscopy, the researchers followed the movement and interaction of HIV-infected cells in the spleen of mice. They watched as infected cells induced contact with uninfected cells, and the uninfected cell would then pause for a time on the infected cell--building a physical connection between them.
Scientists describe these infectious connections as virological “synapses” because they resemble the way that cells of the nervous system or the immune system communicate through intimate cell-to-cell connections.
A mutation factory
The investigators believe the proteins that make up the HIV virion are being assembled at the site of the bridge and then directly moved to the cell being infected. Cell-to-cell infection allows several viruses to simultaneously pass between the connected cells. The researchers found that multiple viruses could infect a single cell through virological synapses.
This pathway allows multiple copies of HIV to transmit together from cell to cell, a genetic property that can help mutant viruses to accumulate. This may help explain the high mutation rate that allows the virus to escape from immune responses, says Mr. Law. “The genetic mixing that happens when a cell is infected with multiple HIV virions can lead to novel genetic recombination that then gets passed into the next immune cell that is infected.”
Co-authors of the study include Alice W. Yewdall, Rebecca K. Lee and Olga L. Herrera, from the Icahn School of Medicine at Mount Sinai; and Dominik Wodarz and Natalia L. Komarova from the University of California, Irvine.
The study was supported by the National Institute on Drug Abuse (F31DA036425, R01AI074420, R01AI093998, and Avant Garde DA028866), the National Institute of General Medical Sciences (GM113885), and Burroughs Wellcome Investigators in the Pathogenesis of Infectious Disease Fund.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, employing 48,000 people across its hospitals and more than 400 outpatient practices, as well as more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
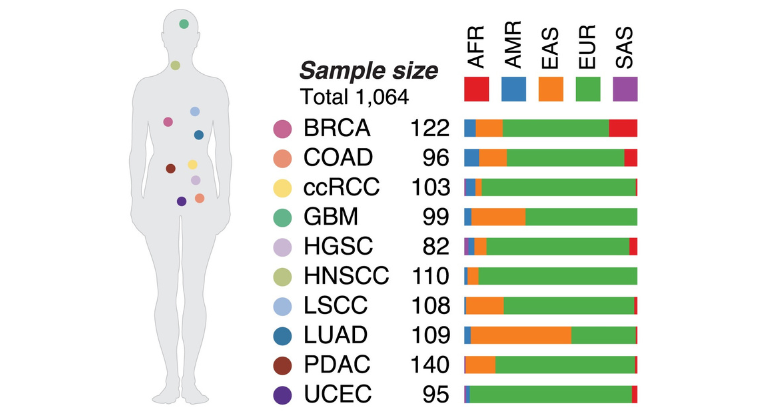
Study Reveals How Inherited Genes Help Shape the Course of Cancer
Apr 14, 2025 View All Press Releases
Mount Sinai Launches AI Small Molecule Drug Discovery Center
Apr 02, 2025 View All Press Releases
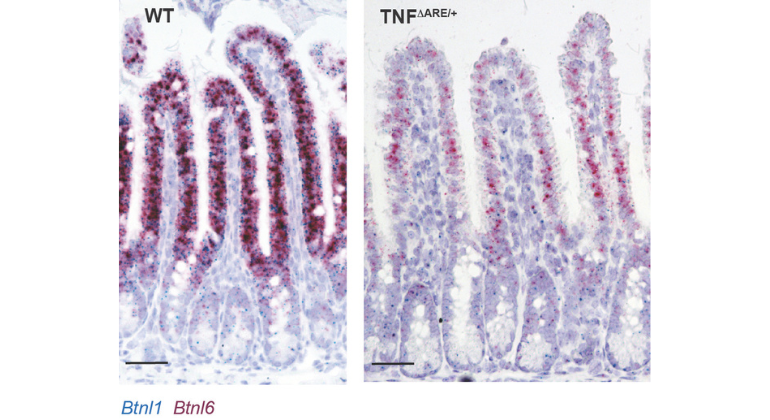
Mount Sinai Researchers Identify Key Gut Sensor That Regulates Digestion and Immunity
Mar 24, 2025 View All Press Releases
Mount Sinai Leads Phase 3 Trial in Myelofibrosis Treatment
Mar 19, 2025 View All Press Releases
Personalized Cancer Vaccine Proves Promising in a Phase 1 Trial at Mount Sinai
Mar 17, 2025 View All Press Releases